Research Article
Laparoscopic partial nephrectomy-does tumor profile influence the operative performance?

Krishanu Das*, George P Abraham, Kishnamohan Ramaswai, Datson George P, Jisha J Abraham, Thomas Thachill and Oppukeril S Thampan
Lakeshore Hospital, Kochi, Kerala, India
*Address for Correspondence: Dr Krishanu Das, Lakeshore Hospital, Kochi, Kerala, India, Email: [email protected]
Dates: Submitted: 20 September 2017; Approved: 09 October 2017; Published: 10 October 2017
How to cite this article: Krishanu D, Abraham GP, Ramaswai K, George PD, Abraham JJ, et al. Laparoscopic partial nephrectomy-does tumor profile influence the operative performance? Arch Surg Clin Res. 2017; 1: 056-060.
DOI: 10.29328/journal.ascr.1001009
Copyright License: © 2017 Krishanu D, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction: Laparoscopic approach is emerging as a standard of care approach for management of masses amenable to partial nephrectomy. Laparoscopic partial nephrectomy is a challenging surgery and its successful performance depends on various factors. We aim to evaluate the influence of tumor characterestics on the operative performance for laparoscopic partial nephrectomy.
Methods: Patients undergoing laparoscopic partial nephrectomy in our institution were recruited for this study. The tumor profile was evaluated by a senior radiologist from cross sectional imaging (computed tomography or magnetic resonance imaging). Tumor characerestics was defined by assessing tumor size, tumor location and RENAL score. The operative performance was evaluated in terms of warm ischemia time, blood loss, operation duration and any significant operative complications. Statistical inference was drawn.
Results: 37 patients who underwent laparoscopic partial nephrectomy between January 2010 and June 2012 were included in this study. The mean tumor dimension was 3.81 cms. 21 tumors involved left kidney and 16 involved right kidney. 12 were located in upper pole, 8 were located in midpole and 17 were located in lower pole. The average RENAL score was 6.56. The mean warm ischemia time, blood loss and operation duration was 26.29 minutes (min), 256.76 millilitres (ml) and 208.11 min respectively. Statistically significant correlation was appreciated between tumor location (polar location, side, anterior/ posterior location) and RENAL score and operative parameters (warm ischemia time and operation duration). Tumor size did not have any correlation with the operative parameters.
Conclusion: The operative performance of laparoscopic partial nephrectomy is significantly influenced by the tumor location and RENAL score.
Introduction
Partial nephrectomy is a well established procedure for management of renal masses, where sufϐicient renal parenchyma can be preserved after complete removal of the kidney tumor [1]. In expert hands, laparoscopic partial nephrectomy has shown comparable oncological outcome and acceptable renal salvage to open partial nephrectomy, with the added advantage of superior morbidity proϐile [2]. Successful performance of laparoscopic partial nephrectomy not only depends on operator skills but also the characterestics of the tumor concerned. Several assessment tools have been proposed in recent literature to help deϐine the tumor proϐile [3-5].Our aim was to assess the inϐluence of these tumor characterestics on our operative performance of laparoscopic partial nephrectomy.
Methods
All patients undergoing laparoscopic partial nephrectomy between January 2010 and June 2012 were included in this analysis. All patients were evaluated in detail including presenting complaints, clinical parameters, blood and renal profile. All patients underwent detailed imaging preoperatively-Computed tomography urogram (CTU) or Magnetic resonance urogram (MRU, if creatinine>1.4 mg/dl). The tumor profile was assessed by a single senior radiologist using standardized criteria [3-5]. The parameters included were tumor size, tumor location, tumor depth. RENAL nephrometry score was assessed from points assigned for Tumor radius, Exophytic/endophytic properties, Nearness to the collecting system, Anterior/posterior location and Location relative to polar lines. The technique of partial nephrectomy was as follows-after colonic mobilisation along the line of Toldt, the dissection was continued along a plane between the Gerotas fascia and the renal capsule all around except the area around the tumor. A cuff of peritumoral fat was preserved. The renal pedicle was then mobilized and the renal artery and vein was clamped en masse using Satinsky clamp applied through an umbiliucal port. The line of resection was point mapped using hook electrocautery keeping a generous margin from the tumor edge. Tumor excision was carried out along this mark using cold scissors. The renal bed was fulgurated using spatula and electrocautery followed by single layer full thickness suturing using No 1 polyglactin. Even in cases of caliceal disruption, single layer full thickness parenchymal renorrhaphy was undertaken without separate calicorrhaphy. No floseal or surgical bolster was applied on the remnant renal bed. The operative profile was recorded in detail. The parameters recorded included warm ischemia time, blood loss, operation duration and any significant intraoperative or postoperative complications. Statistical analysis was carried out using T test, Wilcoxon rank sum test and One way Annova test. A p value <0.05 was remarked as statistically significant.
Results
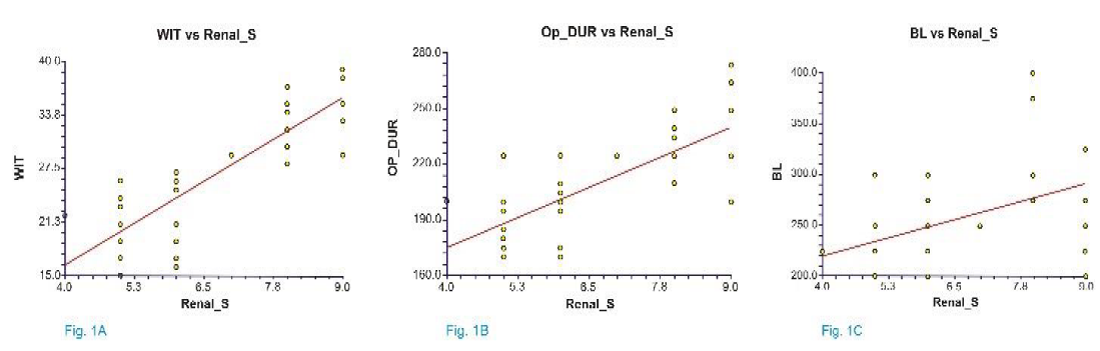
37 patients were included in this analysis. The demographic and tumor profile is highlighted in tables 1,2. The mean±standard deviation RENAL score was 6.56±1.52. One patient experienced significant bleeding after Satinsky clamp release that was managed by additional suturing. One patient required blood transfusion in postoperative period. In seven patients caliceal disruptions during tumor excision were obvious and despite omitting separate calicorrhaphy, none of them experienced any urine leak or prolonged drainage postprocedure. One patient underwent simultaneous laparoscopic partial nephrectomy for solitary right upper pole metastasis in solitary kidney and laparoscopic segmentectomy for solitary segment VII liver metastasis. Postsurgery he suffered from hepatocellular failure and on fifth postoperative day he died. No other major intraoperative or postoperative events were encountered in this patient cohort. The influence of tumor profile on operative parameters is depicted in tables 3,4 and figure 1. Statistically significant associations were observed between tumor location and RENAL score and warm ischemia time and operation duration. Procedural blood loss was not significantly associated with tumor location but with RENAL score. Tumor size had no correlation with operative profile.
| Table 1: Demographic / tumor profile. | |
| Parameter | Value |
| Mean±SD age (range) | 52.02±13.57 years (34-82 years) |
| Gender-male: female | 29:12 |
| Mean±SD BMI (range) | 22.93±1.32 kg/m2 (range 20.8- 25.2 kg/m2) |
| ASA grade | Grade I: 31 Grade II: 10 |
| Mean±SD preop creatinine (range) | 1.10±0.53 mg/dl (0.6-3.2 mg/dl) |
| Mean±SD preop eGFR (range) | 76.91±25.92 ml/min (20-140 ml/min) |
| Tumor laterality | Right-17, Left-24 |
| Tumor location | Upper pole-13, Mid pole-9, Lower pole-22 |
| Mean longitudinal tumor dimension (range) | 3.81±1.21 cms (2.9-10 cms) |
| Table 2: Operative/ postoperative profile. | |
| Parameter | Value |
| Mean±SD warm ischemia time (range) | 26.29±7.55 (15-47 min) |
| Mean±SD blood loss (range) | 256.76±65.36 ml (175-450 ml) |
| Mean±SD operation duration (range) | 208.11±26.49 min (170-265 min) |
| Mean±SD day 1 postop creatinine (range) | 1.43±0.61 mg/dl (0.8-3.8 mg/dl) |
| Mean±SD day 1 postop eGFR (range) | 53.94±15.05 ml/min (17-88 ml/min) |
| Mean±SD time to tolerance of orals (range) | 12.94±4.12 hours (8-20 hours) |
| Mean±SD time to drain removal (range) | 45.94±9.36 hours (36-72 hours) |
| Mean±SD duration of hospital stay (range) | 71.94±9.79 hours (60-96 hours) |
| Mean±SD analgesic (paracetamol) (range) | 1955.88±585.39 mgs (1000-3000 mgs) |
| Significant complications | Death-1 (due to hepatocellular failure at day 5, patient underwent laparoscopic partial nephrectomy+ laparoscopic liver segemntectomy for metastasis in solitary kidney with solitary liver metastasis post contralateral laparoscopic radical nephrectomy) |
| Positive surgical margin | 1 |
| Urine leak/ urinoma (significant pelvicaliceal breach-11) | 0 |
| Table 3: One way Anova comparison of operative profile in relation to polar location of tumor. | ||||||
| Polar Location | Mean WIT (min) | Significance | Mean Blood loss (ml) | Significance | Mean Operation duration (min) | Significance |
| LUP | 26 | 0.00004 | 216.67 | 0.27 | 201.67 | 0.000017 |
| LMP | 30.67 | 266.67 | 211.67 | |||
| LLP | 18 | 245.83 | 175.83 | |||
| RUP | 29.4 | 0.00008 | 310 | 0.17 | 230 | 0.00002 |
| RMP | 36.66 | 283.33 | 263.33 | |||
| RLP | 21.4 | 250 | 195 | |||
| Table 4: Wilcoxon rank sum test and equal variance T test comparison of operative profile in relation to tumor side and location. | ||||||
| Location | Mean WIT (min) | Significance | Mean Blood loss (ml) | Significance | Mean Operation duration (min) | Significance |
| Right | 29.61 | 0.019 | 280.77 | 0.010 | 224.23 | 0.0011 |
| Left | 23.73 | 238.33 | 193.33 | |||
| Anterior | 22.1 | 0.0004 | 220 | 0.025 | 242.4 | 0.0017 |
| Posterior | 35.67 | 295 | 300 | |||
Figure 1: Linear regression plot between renal score and warm ischemia time A: operation duration. B,C Blood loss.
Discussion
Widespread usage of cross-sectional imaging in modern medicine has resulted in a rising incidence in the detection of small renal masses. These patients are both asymptomatic and active and prefer surgeries with limited morbidity. Hence there is an increasing demand for performing partial nephrectomy through laaroscopic approach. Surgeons are also more versed with laparoscopic techniques presently and keen to offer challenging surgeries through minimally invasive approach in suitable patients. Hence there is a global increase in performing laparoscopic partial nephrectomy and the parameters that may influence the outcome of this surgery need to be defined. The focus of our study was to identify these factors. Preoperative identification of unfavorable tumor characterestics will help the surgical team in their preoperative preparartions and necessary steps may be taken to effectively ward of adverse intraoperative happenings. Warm ischemia time, blood loss and procedural complications are important parameters to gauge the procedural complexity for laparoscopic partial nephrectomy. All our procedures were performed obeying the same principle and our operative parameters were comparable to the published literature [6,7]. Recently few scoring systems have emerged to quantitate the tumor characterestics in a standardised pattern [8,9]. In our study we included the RENAL nephrometry score to define tumor profile and assessed the reproducibility of this scoring system. RENAL score had significant correlation with warm ischemia time, blood loss and operation duration. Surgeries were more complex in tumors with higher RENAL scores (>7). This was similar to results from other centers published in literature. Additional inferences from our analysis were-tumors located on the left had more preferable operative profile than right sided tumors, tumors located in the lower pole recorded the lowest warm ischemia time followed by upper polar tumors. Mid polar tumors were the most complex to handle. Hew et al. [9], also reported similar observations in their analysis where mid polar tumors were associated with maximum complications. Additionally, in our study posteriorly located tumors had longer warm ischemia and operative duration than anteriorly located tumors (Tables 5,6).
| Table 5: Equal variance T test comparison of operative profile and renal score ≤ 7 (n=24) vs >7 (n=13). | ||
| Parameter | T score | p |
| Warm ischemia time | -8.5764 | 0.0000 |
| Blood loss | -3.5156 | 0.0006 |
| Operation duration | -6.3103 | 0.0000 |
| Table 6: R-squared value and Strength of correlation between Renal score and operative profile. | |||
| Parameter | Warm ischemia | Blood loss | Operation duration |
| R-squared value | 0.7128 | 0.1767 | 0.5260 |
| Strength of correlation | 0.8443 | 0.4204 | 0.7252 |
This may be explained by the time taken for suturing the remnant renal bed. Our operator was right handed and the different axis of suturing for different tumor locations could be responsible for the differences observed in operative profile with different tumor locations. In comparison to warm ischemia time and operation duration, blood loss had less significant correlation with tumor profile. Although some authors have assessed PADUA scoring and C-index for predicting tumor characterestics, such scoring parameters were not assessed in this study due to complexity of calculation [9,10]. All scoring assessments were done by a single radiologist and all procedures were performed by a single surgeon proficient in laparoscopic exercises. This eliminated the possibility of bias due to interradiologist or intersurgeon differences. In our study tumor characterestics significantly correlated with the complexity of operative performance and meaningful conclusions could be generated. However larger prospective studies including more subjects may be needed to validate these results.
Conclusion
Tumor location (sidedness, polar location, anterior/posterior location) signiϐicantly inϐluences the operative performance of laparoscopic partial nephrectomy. Tumor size has no correlation with the operative proϐile. Additionally, RENAL nephrometry score can accurately predict the operative performance and a more complex procedure may be anticipated with a higher RENAL score.
References
- Campbell SC, Novick AC, Belldegrun A, Blute ML, Chow GK, et al. Guideline for management of the clinical T1 renal mass. J Urol. 2009; 182: 1271-1279. Ref.: https://goo.gl/yPst1a
- Dulabon LM, Lowrance WT, Russo P, William C. Huang. Trends in renal tumor surgery delivery within the United states. Cancer. 2010; 116: 2316-2321. Ref.: https://goo.gl/dWw9vC
- Kutikov A, Uzzo RG. The RENAL nephrometry score: a comprehensive standardized system for quantitating tumor size, location and depth. J Urol. 2009; 182: 844-853. Ref.: https://goo.gl/cAZTvp
- Ficara V, Novara G, Secco S, Macchi V, Porzionato A, et al. Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumors in patients who are candidates for nephron-sparing surgery. Eur Urol. 2009; 56: 786-793. Ref.: https://goo.gl/Q7AKJ5
- Simmons MN, Ching CB, Sampalski MK, Park CH, Gill IS. Kidney tumor location measurement using the C-index method. J Urol. 2010; 183: 1708-1713. Ref.: https://goo.gl/YMAJ81
- Gill IS, Desai MM, Kaouk JH, Meraney AM, Murphy DP, et al. Laparoscopic partial nephrectomy for renal tumor: duplicating open surgical techniques. J Urol. 2002; 167: 469-477. Ref.: https://goo.gl/DNjEDD
- Gill IS, Matin SF, Desai MM, Kaouk JH, Steinberg A, et al. Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol. 2003; 170: 64-68. Ref.: https://goo.gl/bMzNXH
- Hew MN, Baseskioglu B, Barwari K, Axwijk PH, Can C, et al. Critical appraisal of the PADUA classification and assessment of the RENAL Nephrometry score in patients undergoing Partial Nephrectomy. J Urol. 2011: 186: 42-46. Ref.: https://goo.gl/UpAkoJ
- Sampalski MK, Hernandez A, Gill IS, Simmons MN. C-index is associated with functional outcomes after laparoscopic partial nephrectomy. J Urol. 2010; 184: 2259-2263. Ref.: https://goo.gl/mrrH5Z
- Waldert M, Waalkes S, Klatte T, Markus A. Kuczyk, Peter Weibl, et al. External validation of the preoperative anatomical classification for prediction of complications related to nephron-sparing surgery. World J Urol. 2010; 28: 531-535. Ref.: https://goo.gl/BL3NAa