Research Article
Safety and effectiveness of laparoscopic management in 210 patients with erosion of adjustable Gastric banding

Ramiro Galvez-Valdovinos*, Juan francisco Funes-Rodriguez, Ernesto Marin Y Santillan, Gustavo López Ambriz and Juan Francisco Ramirez-Arias
Bariatric Surgery Service and Laparoscopic Surgery, Hospital Angeles Leon, Mexico
*Address for Correspondence: Ramiro Gálvez-Valdovinos, Bariatric Surgery Service and Laparoscopic Surgery, Hospital Angeles Leon, Av. Cerro Gordo 311-830, Col. Lomas del Campestre, CP 37150, León Guanajuato Mexico, Tel: 52(477)7885683; Email: [email protected]; [email protected]
Dates: Submitted: 13 November 2017; Approved: 20 November 2017; Published: 21 November 2017
How to cite this article: Galvez-Valdovinos R, Funes-Rodriguez JF, Santillan EMY, Ambriz GL, Ramirez-Arias JF. Safety and effectiveness of laparoscopic management in 210 patients with erosion of adjustable Gastric banding. Arch Surg Clin Res. 2017; 1: 077-082.
DOI: 10.29328/journal.ascr.1001013
Copyright License: © 2017 Valdovinos RG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Band erosion; Band erosion management; Gastric band complications; Gastric band revisional surgery; Laparoscopic adjustable gastric banding
Abstract
Background: The band erosion (BE) is defined as the partial or complete movement towards the lumen of the stomach, is also known as migration, gastric incorporation and gastric inclusion. The presentation of this complication involves failure of bariatric procedures being ineffective and consequently requires the removal of the laparoscopic adjustable gastric banding (LAGB), usually through laparoscopic surgery.
The objective of this study is to describe the clinical presentation, diagnostic methods, surgical procedure, postoperative evolution in the integral treatment of BE. Material and Methods: We captured the data of patients with BE since January 2010 to October 2017. Database included the year of patient care, age, and sex, BMI before band placement, percentage of excess weight loss, number of device adjustments, clinical data and surgical procedure performed for resolution.
Results: A total 379 LAGB complications were diagnosed in our Institution; 210 patients with BE were diagnosed and treated, the average age was 39 years; range from 19 to 66 years, sex was 178 women and 32 men. The diagnosis was endoscopic in the 210 patients (100%). The surgical procedure to solve the problem was: to remove the LAGB, the fistulous orifice was closed and patch of omentum. The hospital stay was 3-5 days. The motility was zero. Complications were minor in 3% of the 210 patients (fever, atelectasis, wound infection). One patient was re-operated for evolving to residual abscess.
Conclusions: The BE is a serious failure in bariatric surgery. The resolution in this group of patients was to remove the band, direct closure of the fistulous orifice with patch of omentum. The surgical technique that was performed in this complication is safe, effective and easily reproducible.
Introduction
Inserting a LAGB is simple and effective for controlling obesity in its early stages; however, over the time, many of these patients present complications of the procedure [1]. The current failure rate reported goes from 30 to 70% in studies with follow-up at 13 and 15 years [1,2]. This bariatric procedure has a 3% morbidity rate in the early postoperative stage [2,3] and a 12% morbidity rate in the late postoperative period, with mediocre long-term results. LAGB is a technique used by specialized groups around the world [4,5] when the percentage of excess weight loss does not exceed 45-50% long-term, or when the patient presents an unacceptable quality of life (maladaptive eating and vomiting), such medical treatments are considered failures. The exact causes of LAGB failure are difficult to establish and are based on observational studies. It is likely that the type of LAGB influences the incidence of injuries on the stomach. What is clear is that the learning curve [6], the surgical technique used, [7-9] and care in handling tissues when inserting the LAGB play important roles in avoiding complications [8,9]. Erosion occurred in 1 percent of patients in the LAP-BAND® FDA clinical trial [10]. The presentation is not exact, in the international literature the revision procedures or those made during the learning curve are usually omitted in the publications. In our region of the Country (Mexico) it is estimated that approximately 20,000 gastric band placements have been performed in the last 10 years; our surgical team does not perform gastric banding, it is dedicated to resolve complications of gastrointestinal surgeries of any kind, within of them, we report our experience with 379 complicated cases of LAGB, of which 210 patients presented gastric erosion produced by the gastric band.
Material and Methods
We have received a large number of complications secondary to the LAGB. From January 2010 to October 2017 were treated 379 patients with a complication derived from the LAGB. Within the most frequent late complications in this group of patients was the BE (55.4%). Clinical records were reviewed and the following information was entered in a database: the year of patient care, age, sex, body mass index (BMI) of presenting patients when the LAGB was inserted, the percentage of excess weight loss with LAGB, number of adjustments for LAGB and postoperative complications.
Results
From January 2010 to October 2017 were treated 210 patients with BE, the middle ages was 39 years (range 19 to 66 years), there were 178 women and 32 men. The BMI of patients at the time of placing the LAGB was 40.1 (average) with a range of 39.9-43.6. The percentage of weight loss with the LAGB was in the 30%-41% range with an average of 39%. The elapsed time since the LAGB was placed at retirement time was 13 months to 120 months (Table 1). Patients were comprehensively assessed preoperatively by the surgeon, internist, and anesthesiologist, and preoperative studies according to individual physical condition of each patient. The symptoms were vomiting in 210 patients (100%), dysphagia in 184 patients (87.6%), insufficient weight loss in 172 patients (81.9%), pain and hyperemia port setting as the initial symptom in 90 patients (42.8%), gastro esophageal reflux in 46 patients (21.9%,), abdominal pain in 39 patients (18.5%) and upper digestive bleeding in 27 patients (12.8%). We usually performed pre-operative gastroscopy in all patients with BE, other diagnostic tests used were; upper GI X-ray series was made in 207 patients (98.5%), CT-scan was performed in 172 patients (81.9%). An interesting aspect was the degree of anxiety and depression in this patient group was very high in 205 patients (97.6%).
Table 1: Demographic data of patients with gastric erosion caused by adjustable banding. |
|
| Demographics data | Results |
| Mean age | 39 years (R:19-66) |
| Sex | Women 178 and Men 32 |
| BMI at the time of inserting the LAGB | Mean 40.1, Rank 39.9-43.6. |
| Percentage of weight loss | Mean 39%, Rank 30%-41% |
| Weight gain at 12 months after removal of the LAGB | 100% |
| Gastric band type | Swedish Adjustable Gastric Band (89%), Lap-Band (9%)% and other 2% |
| Number of adjustments before device retirement | 4–11 |
| Time LAGB lasted | 13 –120 months |
Surgical technique
The patient is placed supine with the hips abducted, and monitors are positioned towards the patient head. Pneumoperitoneum is established with a Veress needle at the left costal margin. After all ports are set, the surgery table is placed into reverse Trendelenburg position, the surgeon stands between the patient’s legs, and the assistant is located at the patient’s left side. The procedure begins by dissecting, with a monopolar hook, of adhesions caused by the previous LAGB. To get to the band, which is covered by adhesions, it is more feasible to continue the connection tube and pull it up to the buckle (Figure 1). The buckle of the band is easily identified and a cut on its weak part permits removal of the band. We applied some stitches with nonabsorbable suture 2/00 (EtibondR) on the damaged gastric wall (gastrography) and putting in loose intracorporeal stitches followed by a patch of omentum (Figure 2). All procedures were done by laparoscopy. All patients had a suction Jackson Pratt drain closed. On the second day of the surgery, a water-soluble contrast upper GI X-ray series was made. No patient had fistulas or leaks. On the third day they were given a clear liquid diet, and oral nutritional support was started. The hospital stay was 3-5 days. Postoperative complications were; fever in two patients, atelectasis in two patients and wound infection in the access port in two patients. One patient was reoperated on the third day to drain a secondary abscess to intra-abdominal infection in the surgical wound where it was placed in the LAGB adjustment port. Mortality in this group of patients was zero. In the follow-up of these patients all returned to their original weight. Patients who have accepted another bariatric procedure are recommended to perform it one year after removal of LAGB.
Figure 1: The image shows the moment to discover the belt buckle, once identified, a cut in its weak part permits remove of the band.
Figure 2: The image of the surgery shows the reinforcement of the patch with omentum on the closing of the fistulous orifice.
Figure 3: Patient with erosion; the band has a small bowel fistula, which necessitated intestinal resectioning.
Figure 4: Patient with erosion; the band has a significant collection of cutaneous fistulas, which necessitated resectioning of the greater omentum and a fistulectomy.
Discussion
The industry marketing the LAGB started in the 1990s, creating massive advertising campaigns aimed at scientific congresses of surgical societies. They gave concessions and training to politically well-established surgeons. Only a small group was in charge of LAGB surgeries, and on some occasions they advised and trained other surgeons around the country, who flocked on weekends to our cities. Initially, without an established protocol, they conducted a large number of LAGB procedures, and in many cases the patient was lost in the middle of the marketing push with no expert surgeons to do this bariatric procedure. As a result, the rush to conduct so many operations led to logical complications and lawsuits.
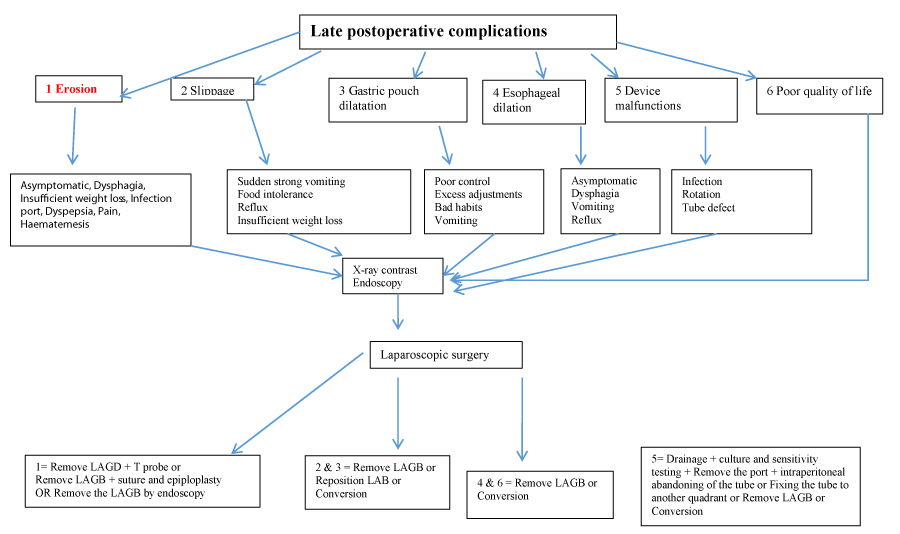
Laparoscopic application of a LAGB is the least invasive method within bariatric procedures and is considered to be the safest. It has the advantage of being a potentially reversible, easy to reproduce procedure. Still, morbidity and poor results in the percentage of weight loss continues to be LAGB bariatric procedures, which comprise 26% of total worldwide bariatric surgery [1-3]. Evidence is present of long-term complications after insertion of an AGB [4]. Approximately 50% of patients who had a LAGB require re-intervention [5]. Early morbidity (30 days) is at 3% [3] and late morbidity (after 30 days) occurs in 12% of patients. We usually use (algorithm #1) that we show to treat late complications. Mortality remains close to 0% in most series; however, these percentages are increasing with the passage of time [6,7]. The BE is a rare complication after LAGB with a reported incidence rate of 1.46 % and the development is usually stealthy and silent. Generally the symptoms of BE are benign, they are not urgent and not life threatening. Paralytic ileus or sepsis is rarely present, however every day new cases of critically ill patients are published [11,12]. The BE normally goes unnoticed for a long period of time because the fibrous capsule seals the band and the connector tube creating adhesions from the peritoneal cavity to the reservoir. The BE should be suspected when in adjustment a cloudy or yellowish liquid can be extracted. We were able to observe cascading signs in the upper GI X-ray series when a percent greater than 60% of the band was inside the stomach. The CT-scan provided interesting data in patients with intestinal obstruction, migration to the small intestine or large intra-abdominal collections, especially for the surgical strategy that would be carried out (Figures 3,4). The gastroscopy showed us the state of the esophageal mucosa, the perfect location of the band, the percentage of intra-gastric migration and the lesions of the gastric mucosa. The experts report endoscopic removal of the LAGB, but that requires the buckles of the band to be eroded and special endoscopic instruments; also, the endoscopist has to be experienced [13-15]. In our group of patients, we attempted to remove the band in three patients with the endoscope, but removal was not possible. When performing laparoscopy and endoscopy together, we discovered that tissue had grown into the buckle of the band, making gastrointestinal endoscopic extraction unachievable. The condition is that 100% of the band is hanging inside the stomach including the buckle. The possible causes of BE are gastric tight sutures, chronic ischemic tissue damage, contamination or infection of the band, an adjustment port infection immediately after surgery, injuries of the gastric wall dissection, and excessive band filling. The BE risk appears to be minimized with plication of the stomach with pars flaccida [16] to cover the band without tension and to ensure that the buckle is free; also it is recommended to treat all infections of the port early on. Of all possible recommendations [17-19] to avoid this very serious complication, we would advise counseling patients to opt for different LAGB bariatric procedures. Surgeons who have treated this complication have faced challenges involving reoperation, the failure of a bariatric procedure, possible postoperative complications, the deteriorating psychological state of the patient, the claims of relatives, being singled out in the hospital corridors by colleagues, discrediting by society, and the height of these challenges, lawsuits.
Algorithm #1: This algorithm grouped the six most frequent complications presented our patient groups. They all lead to surgery. Laparoscopic surgery is the first line of treatment. Treatment options for each complication are based on recommendations contained in the literature*.
Conclusions
The BE is a serious failure in bariatric surgery. The resolution in this group of patients was to remove the band, direct closure of the fistulous orifice with patch of omentum. The surgical technique that was performed in this complication is safe, effective and easily reproducible.
References
- Sertkaya M, Emre A, Yazar ME, Bülbüloğlu E. Diagnosis and management of early gastric band slip after laparoscopic adjustable gastric banding. Wideochir Inne Tech Maloinwazyjne. 2016; 11: 121-125. Ref.: https://goo.gl/Ux4WK7
- Smith MD, Patterson E, Wahed AS, Belle SH, Berk PD, et al. Thirty-day mortality after bariatric surgery: independently adjudicated causes of death in the longitudinal assessment of bariatric surgery. Obes Surg. 2011; 21: 1687-1692. Ref.: https://goo.gl/WyXiSQ
- Nguyen NT, Hohmann S, Nguyen XM, Elliott C, Masoomi H. Outcome of laparoscopic adjustable gastric banding and prevalence of band revision and explantation at academic centers: 2007-2009. Surg Obes Relat Dis. 2012; 8: 724-727. Ref.: https://goo.gl/e5RA96
- Carelli AM, Youn HA, Kurian MS, Ren CJ, Fielding GA. Safety of the laparoscopic adjustable gastric band: 7-year data from a U.S. center of excellence. Surg Endosc. 2010; 24: 1819-1823. Ref.: https://goo.gl/gmDNp5
- Chapman AE, Kiroff G, Game P, Foster B, O’Brien P, et al. Laparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature review. Surgery. 2004; 135: 326-351. Ref.: https://goo.gl/CR5qFX
- Niville E, Dams A, Vlasselaers J. Lap-Band erosion: incidence and treatment. Obes Surg. 2001; 11: 744-747. Ref.: https://goo.gl/gF3VgU
- Dang JT, Switzer NJ, Wu J, Gill RS, Shi X, et al. Gastric Band Removal in Revisional Bariatric Surgery, One-Step Versus Two-Step: a Systematic Review and Meta-analysis. Obes Surg. 2016; 26: 866-873. Ref.: https://goo.gl/5Th75s
- Garg T, Rosas U, Rivas H, Azagury D, Morton JM. National prevalence, causes, and risk factors for bariatric surgery readmissions. Am J Surg. 2016; 1: 76-80. Ref.: https://goo.gl/CKcngK
- Himpens J, Cadière GB, Bazi M, Vouche M, Cadière B, et al. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011; 146: 802-807. Ref.: https://goo.gl/cJVFcJ
- Rubenstein RB. Laparoscopic adjustable gastric banding at a U.S. center with up to 3-year follow-up. Obes Surg. 2002; 12: 380-384. Ref.: https://goo.gl/wZWoqk
- Reche F, Mancini A, Faucheron JL. Gastric Band Migration Causing Jejunal Obstruction: a Life-Threatening Complication. J Gastrointest Surg. 2017; 4: 10. Ref.: https://goo.gl/vG9Hhp
- Rudd AA, Lall C, Deodhar A, Chang KJ, Smith BR. Gastropericardial Fistula as a Late Complication of Laparoscopic Gastric Banding. J Clin Imaging Sci. 2017; 7: 3. Ref.: https://goo.gl/E8ok5W
- Spann MD, Aher CV, English WJ, Williams DB. Endoscopic management of erosion after banded bariatric procedures. Surg Obes Relat Dis. 2017; 13: 1875-1879. Ref.: https://goo.gl/QcMj8Y
- Dogan ÜB, Akin MS, Yalaki S, Akova A, Yilmaz C. Endoscopic management of gastric band erosions: A 7-year series of 14 patients. Can J Surg. 2014; 57: 106-11. Ref.: https://goo.gl/rm8Zvh
- Basa NR, Dutson E, Lewis C, Derezin M, Han S, et al. Laparoscopic transgastric removal of eroded adjustable band: a novel approach. Surg Obes Relat Dis. 2008; 4: 194-197. Ref.: https://goo.gl/epUQSU
- Di Lorenzo N, Furbetta F, Favretti F, Segato G, De Luca M, et al. Laparoscopic adjustable gastric banding via pars flaccida versus perigastric positioning: technique, complications, and results in 2,549 patients. Surg Endosc. 2010; 24: 1519-1523. Ref.: https://goo.gl/YPsMCk
- Carelli AM, Youn HA, Kurian MS, Ren CJ, Fielding GA. Safety of the laparoscopic adjustable gastric band: 7-year data from a U.S. center of excellence. Surg Endosc. 2010; 24: 1819-1823. Ref.: https://goo.gl/UBHwXN
- Eid I, Birch WD, Sharma MA, Sherman V, Karmali S. Complications associated with adjustable gastric banding for morbid obesity: a surgeon’s guides. Can J Surg. 2011; 54: 610-66. Ref.: https://goo.gl/QJ2mGy
- Egberts K, Brown WA, O'Brien PE. Systematic review of erosion after laparoscopic adjustable gastric banding. Obes Surg. 2011; 21: 1272-1279. Ref.: https://goo.gl/SigGLa