Research Article
Scrotal Hydroceles not associated with Patent Processus Vaginalis in Children

Masao Endo1*, Fumiko Yoshida1, Masaharu Mori1, Miwako Nakano1,Toshiya Morimura2, Yasuharu Ohno2 and Makoto Komura2
1Department of Pediatric Surgery, Saitama City Hospital, Japan2Department of Pediatric surgery, Saitama Medical University, Japan
*Address for Correspondence: Masao Endo, Department of Pediatric Surgery, Saitama City Hospital, 1-16-18, Higashiyaguchi, Ota-ku, Tokyo, 146-0094, Japan, Phone & Fax: +81-3-3732-3500; E-mail: [email protected]
Dates: Submitted: 18 April 2018; Approved: 30 April 2018; Published: 02 May 2018
How to cite this article: Endo M, Yoshida F, Mori M, Nakano M, Morimura T, et al. Scrotal Hydroceles not associated with Patent Processus Vaginalis in Children. Arch Surg Clin Res. 2018; 2: 005-012. DOI: 10.29328/journal.ascr.1001015
Copyright License: © 2018 Endo M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: After the closure of patent processus vaginalis (PPV) in boys with indirect inguinal hernia (IIH) or hydrocele, large scrotal hydroceles can occur on rare occasions despite the complete occlusion of internal inguinal ring (IIR). We present some cases that may help to explain the cause of this rare occurrence.
Materials: During last 14 years, six boys exhibited non-communicating large scrotal hydroceles (2 right, 1 left, 3 bilateral) among 352 children who underwent laparoscopic repair for hydroceles. Ages ranged from 7 months to 15 years with a median of 12 years. Five of them had a history of repair for hydrocele or IIH prior to the definitive surgery and one boy underwent an initial operation.
Results: In all the patients, laparoscopic inspection at the definitive surgery revealed completely closed IIRs. One infant with primary hydroceles was found to have large hydroceles bulging into the peritoneal cavity. All the patients were treated with subtotal removal of the sac without any recurrence. Marked thickness of the sack walls with abundant lymph vessels was characteristic histopathological findings.
Conclusions: The complete occlusion of the PPV does not always prevent the recurrence of hydrocele through alternative pathogenesis. The pathological findings of resected specimens suggested a disturbance in lymph flow in the testicular system. The subtotal removal of the sac is the treatment of choice. Diagnostic laparoscopy prior to a direct cut-down approach to the neck of the seminal cord is advisable to identify non-communicating hydroceles to avoid further impairment of lymph drainage around the IIR.
Introduction
Scrotal hydrocele in boys older than 4 months of age is thought to represent the entrance of peritoneal fluid into the scrotal portion of a patent processus vaginalis (PPV), suggesting an alternative manifestation of an indirect inguinal hernia (IIH), and the ligation of the PPV at the internal inguinal ring (IIR) is regarded as the treatment of choice [1]. On rare occasions, however, we have observed large scrotal hydrocele appearing postoperatively after the closure of the PPV in boys with IIH or hydrocele, despite the complete occlusion of the IIR. Here, we present findings that may help to explain the possible causes of this rare occurrence. The purpose of this paper is to introduce our experience in treating this rare occasion and to discuss its etiology and treatment.
Materials and Methods
During last 14 years, six boys exhibited large scrotal hydroceles not associated with PPV among a sequential series of 352 children who underwent laparoscopic repair for hydroceles. The patient list is shown in table 1. The patient ages ranged from 7 months to 15 years with a median age of 12 years. The location of the hydrocele was right in 2, left in 1 and bilateral in 3 patients. The medical records of the children were analyzed to investigate the previous history, the operative findings and procedure, and the pathological findings of the resected wall of the hydrocele.
| Table 1: Patient list | |||||||
| No. | Name | Age | Site | Previous morbidity | Previous operation | Associated morbidity | Final operation |
| 1 | S.W. | 7m | Bilateral | High scrotal testis (bilat) | Subtotal hydrocelectomy + TSO (bilat) |
||
| 2 | Y.K. | 2y9m | Left | Hydrocele (lt) | Laparoscopic repair (1y11m) | High scrotal testis (lt) | Subtotal hydrocelectomy + TSO (lt) |
| 3 | N.S. | 11y | Bilateral | Indirect hernia (bilat) Hydrocele (bilat) |
Laparoscopic repair (1y) Hydrocelotomy (10y) |
Subtotal hydrocelectomy (bilat) | |
| 4 | N.F. | 13y | Bilateral | Hydrocele (bilat) | Cut-down repair (1y) | Subtotal hydrocelectomy (bilat) | |
| 5 | Y.I. | 15y | Right | Hydrocele (rt) | Cut-down repair + hydrocelotomy (15y) |
Wilms' tumor (6y)* | Subtotal hydrocelectomy (rt) |
| 6 | T.M. | 15y | Right | Hydrocele (lt) | Cut-down repair (3y) | Lateral cervical fistula (3y)** Allergic purpura (6y) Suspected orchiditis (15y) |
Subtotal hydrocelectomy (lt) |
Case Presentation
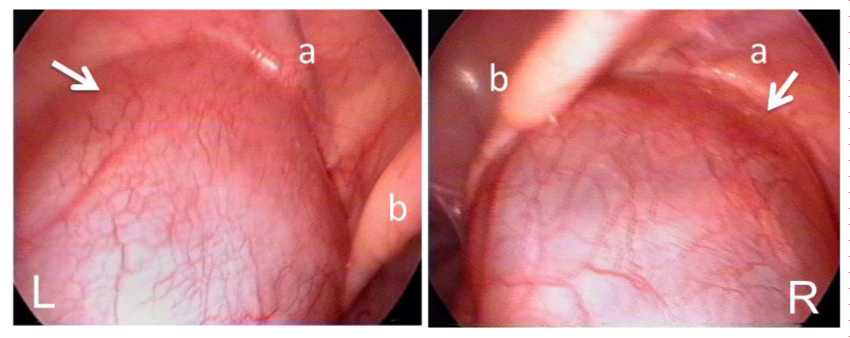
Patient 1 (S.W.): A 7 month-old male infant developed large bilateral hydroceles one month after birth (Figure 1). Clear straw-colored fluid (100 ml from the right side and 80 ml from the left, respectively) was aspirated after the puncture of each hydrocele. Rapid re-accumulation of the fluid during 2 or 3 days conducted to undergo early stage operation. Diagnostic laparoscopy revealed large hydroceles bulging into the peritoneal cavity (Figure 2). No PPV was found after evacuation of the fluid by aspiration of 45 ml from the right side and 70 ml from the left, respectively. No intraperitoneal effusion was noted.
Figure 2: Pt.1 (S.W.), Huge hydroceles protruding into the peritoneal cavity at bilateral IIRs (arrows). Abbreviations: a, inferior epigastric vessels; b, medial umbilical fold.
Trans-scrotal incision was done and the tunica vaginalis thickened up to approximately 2~3 mm in thickness was removed leaving the testicular bed. Both testicles, which located at the high-scrotal position, were relocated to the bottom of the scrotum by elongating the stalk after dissecting the connective tissue around the testicular vessels and the spermatic cord high at its neck. Because the testicular arteries and the spermatic cord were buried in the thickened tunica vaginalis, transillumination was applied to identify them. The surgical specimen was not sent to the laboratory. Postoperative massive edema on bilateral scrotum subsided gradually during next several months. No swelling has appeared thereafter.
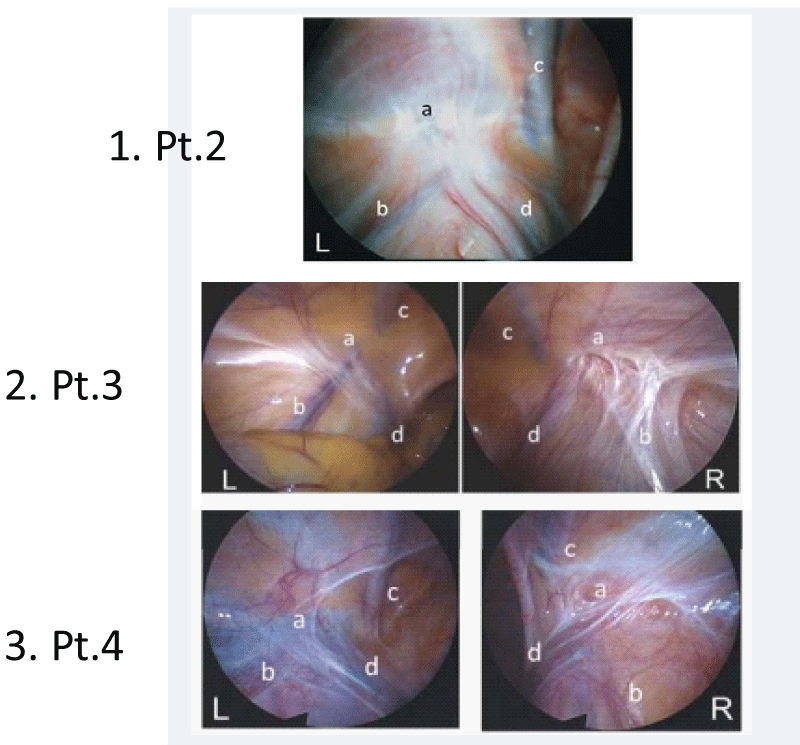
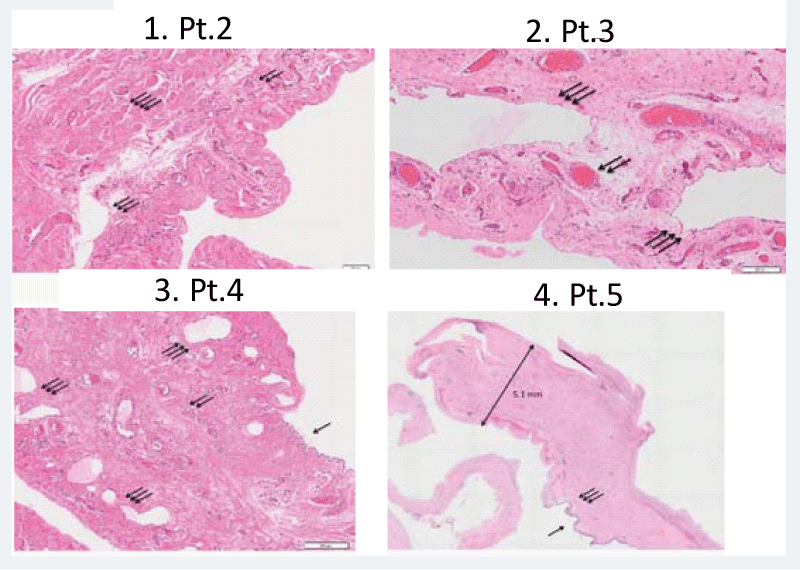
Patient 2 (Y.K.): A two year and 9 month old boy exhibited recurred hydrocele at the left side. He underwent laparoscopic percutaneous extraperitoneal repair [2] for left hydrocele with PPV at the age of one year and 11 months. Right IIR was found to be obliterated. The large hydrocele developed soon after the operation showing no tendency to spontaneous regression. At the second-look operation, diagnostic laparoscopy revealed closed IIR with thick cicatricial tissues (Figure 3.1). Because preoperative sonography revealed the testis located in a high scrotal region, trans-scrotal orchiopexy was done after resection of the thickened tunica vaginalis [3]. Histological examination showed thickened tunica vaginalis, containing partially cremaster muscle fibers, with proliferated lymph vessels (Figure 4.1).
Figure 3: Representative laparoscopic findings of IIRs at the definitive surgery. 1. Pt.2 (Y.K.), 2. Pt.3 (N.S.), 3. Pt.4 (N.F.), The IIRs of the affected side showed various types in the spectrum of the morphological findings of closed IIRs [17]; type “flat”, covered with thin cicatricial tissue resembling congenitally obliterated IIR (left IIR of Pt.3 and 4), type “dimple”, having thick cicatricial tissue and a dimple at the center (right IIR of Pt.4), and type “convergence”, covered with thick cicatricial tissues gathering in the center of depressed IIR (left IIR of Pt.2 and right IIR of Pt.3). Abbreviations: a, IIR; b, testicular vessels; c, inferior epigastric vessels; d, spermatic duct.
Figure 4: Representative histopathological findings of the hydrocele wall (H&E original magnification x 100). 1 Pt.2 (Y.K.), Thickened hydrocele wall containing dilated lymph vessels and cremaster muscle fibers. 2 Pt.3 (N.S.), Proliferation of markedly dilated lymph vessels. 3 Pt.4 (N.F.), A wall lined by flattened mesotherial cells, containing proliferated blood vessels and lymph vessels. Neutrophil infiltrations are scattered. 4 Pt.5 (Y.I.), Loupe magnification showing a thickened tunica vaginalis wall, reaching up to 5.1 mm in thickness, with dense connective tissue. Most of mesothelial linings are degenerated and falling. Abbreviations: arrow, mesothelial linings; double arrow, blood vessels; triple arrow, lymph vessels; fourfold arrow, cremaster muscle fibers.
Patient 3 (N.S.): A 11 year-old boy appeared with bilateral large hydroceles after second-look operation for bilateral hydroceles that developed 9 years after laparoscopic repair for bilateral indirect inguinal hernia at the age of one year. At the 2nd-look operation, ninety ml of straw-colored fluid was aspirated from the right hydrocele. Because the cut-down procedures could not reach to the neck of the hydrocele for dense cicatricial tissue, only wide hydrocelotomy was done for bilateral sacs. But reaccumulation of the fluid developed soon after and persisted for one year.
Diagnostic laparoscopy at the definitive surgery revealed completely closed IIR (Figure 3.2). The right testicular artery was involved in thick cicatricial tissue and seemed to wither in comparison with the left side. The right testicle was found to develop to approximately half size of the left side. Subtotal resection of the markedly thickened tunica vaginalis on both sides were performed. Dilated lymph vessels were seen along the inner surface. Histology of the resected sac revealed marked thickness of the wall with proliferation of remarkably dilated lymph vessels (Figure 4.2).
Patient 4 (N.F.): A 13 year-old boy developed large hydroceles on bilateral side 12 years after a cut-down repair for bilateral hydroceles. Diagnostic laparoscopy revealed completely closed IIR in both sides (Figure 3.3). No abnormal peritoneal fluid accumulation was noted. The hydroceles were fist-sized, tense and saccular in form and were full of straw-colored serous fluid. The tip of the sac extended toward the IIR, but no connection to the peritoneal cavity was observed.
The tunica vaginalis was approached through a trans-scrotal incision, and was excised at its base with trimming along the spermatic cord. The testis and epididymis within the sac were grossly normal. Postoperative course was associated with massive scrotal edema on both sides, which spontaneously improved after several weeks. Histological examination revealed a thickened wall lined by flattened mesotherial cells, containing proliferated vessels and lymph vessels. Neutrophil infiltrations were scattered (Figure 4.3).
Patient 5 (Y.I.): A 15 year-old boy exhibited a fist-sized and tense swelling in the right hemiscrotum that had persisted for one year. He had a history of nephroblastoma originated in the isthmus of the horse-shoe kidney at the age of 6 years, which was extirpated with peri-aortic lymph node dissection. Cut-down repair with high ligation of rudimentary processus vaginalis with hydrocelotomy was performed. Straw-colored clear fluid gushed out when the hydrocele was cut.
A large hydrocele reappeared soon after the operation. At the time of a re-operation, performed 3 months later, a closed IIR was laparoscopically observed, prompting us to perform a subtotal hydrocelectomy. Marked edema with thickness of the connective tissue around the right testis persisted for several months, but the edema gradually improved and no further recurrences occurred. Histological study of the resected sac revealed a thickened tunica vaginalis wall with dense connective tissue with scattered lymph vessels. Most of mesotherial linings are degenerated and exfoliated (Figure 4.4).
Patient 6 (T.M.): A 15 year-old boy, with a history of cut-down repair for left hydrocele at the age of three years, left second branchial cleft remnant that was extirpated at the same session and allergic purpura at the age of six years, developed a painful swelling of the right hemiscrotum. An echogram showed a peri-testicular hyper-echogenic structure with the accumulation of fluid containing debris. The pain subsided after several days of antibiotics treatment, but the fluid accumulation persisted. Diagnostic laparoscopy revealed completely closed IIR. Subtotal resection of the tunica vaginalis sac that contained straw-colored clear fluid was done through skin crease incision. The testis and epididymis were looked normal. The resected specimen was not sent to a laboratory.
Discussion
The treatment of scrotal hydroceles, typically in association with a connecting PPV, is very common in pediatric surgery. Non-communicating hydroceles, which develop in newborns as a result of peritoneal fluid that has become trapped in the scrotum portion of the PPV, disappears over a period of several months after the spontaneous obliteration of the IIR. Recurrent hydroceles that occur after an operation for IIH are also usually associated with a recanalized IIR.
In 1998, we experienced the large hydrocele without any communication with peritoneal space as the first case. Thereafter, we could accumulate 6 similar cases among a consequent series of 352 children with hydrocele.
Ein SH et al. reported five boys who developed very large recurrent postoperative scrotal hydroceles after pediatric inguinal hernia repair as a rare complication, which had never been reported before [4]. The features reported by Ein’s group were similar to those of the presently reported series with a few exceptions; a histopathological examination revealed the marked degeneration of the sack wall in our series unlike the negative results reported by Ein’s group, and one patient with primary hydrocele in young infant was included in our series, which has not been reported in previous literatures. Considering these rare occurrences, hydroceles in adolescents and adults are likely to have been identified as idiopathic hydroceles [5,6]. Wilson JM et al., reported a high possibility of non-communicating hydroceles in boys older than 12 years of age [7].
Regarding the etiology of idiopathic hydrocele, this topic was debated in the 1940s – 1950s without any definitive conclusion being reached [8], because hydrocele cases associated with a PPV were not discriminated from those that were not associated with a PPV. Fluid accumulation was thought to be induced because of a failure in lymphatic absorption, and the subsequent thickening of the sack wall was thought to prevent absorption further.
The proposed pathogenetic mechanism was examined by performing a lymphography of the testis and its adnexa (tunica vaginalis, epididymis and tissue near the vas deferens) [9]. In some patients with idiopathic hydrocele, the normal lumbar pathway was absent and drainage to the iliac lymph nodes was not observed in all the patients. Consequently, a possible cause of idiopathic hydrocele may include excessive secretion within the testicular tunics concomitant with a decreased reabsorption because of the absence or malfunction of the efferent lymphatics. Postvaricocerectomy hydrocele is well-known complication, when the mass ligation and division of the spermatic cord applied [10].
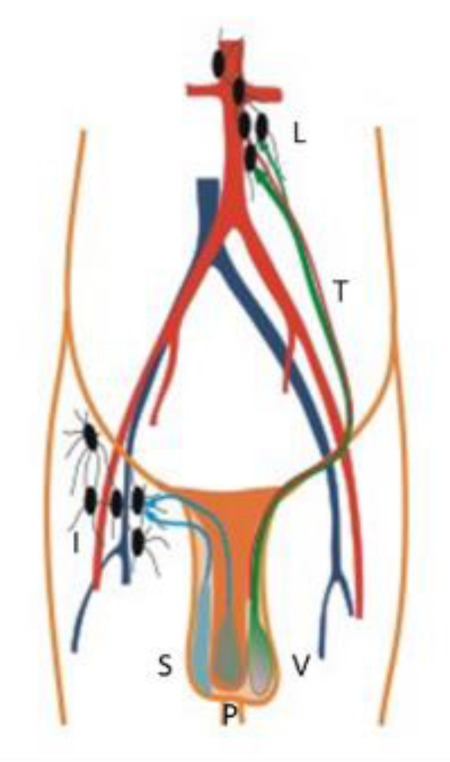
During the fetal life, the testicle originates at the retroperitoneal space near the kidney, and descends into the scrotum along with the testicular artery and lymphatic system. So, lymphatic drainage of the testis follows the testicular arteries back to the paraaortic lymph node group, while lymph from the scrotum and the penis drains to the inguinal lymph nodes (Figure 5).
Detailed histopathological reports of the hydrocele wall have been scarce in previous literature even in textbooks of urology and surgical pathology. Usually, normal tunica vaginalis is a serous membrane consisted of thin collagen fibers covered by a layer of simple squamous mesotherial cells. The wall of primary hydroceles is of this membrane.
In our series, histopathological studies of the resected sacks were macroscopically found to be markedly hypertrophied and edematous with a thickness of up to 2 - 5 mm. Microscopic findings revealed a markedly thickened tunica vaginalis lined by flattened or cuboidal mesotherial cells along the inner surface, and mostly thick collagen fibers on the parietal side. The walls exhibited nonspecific chronic inflammation with neutrophil infiltration and lymphectasia. Markedly dilated lymph vessels were present spottily. Our description may be the first to address lymphectasia and the proliferation of dilated lymph vessels in the wall. These findings suggest that lymph drainage from the testicular system is disturbed at some point proximal to the parietal tunica vaginalis.
Known etiology of fluid accumulation in the vaginal sac are; inflammatory conditions such as epididymitis/ orchiditis, torsion of appendix testis, omental plug at the IIR, testicular torsion, tumors, parasitic infection, ascites, and post-varicocele fluid collection [11]. None of above condition was noted in our cases except suspected orchiditis in Pt. 6. Concerning the etiology, Pt.5 underwent paraaortic lymph node dissection during the removal of the Wilm’s tumor. Pt.6 had possible orchiditis prior to the hydrocele development, but the fluid accumulation persisted after subsiding of the inflammatory process. Pt.3 showed thick cicatricial tissue at the IIR with the withered testicular artery. Another two patients also showed some cicatricial tissue at the IIR in diagnostic laparoscopy prior to the definitive surgery, but their proximal portion of the spermatic cord seemed to be intact. Two patients had associated maldescended testicle. One patient had an episode of allergic purpura.
The variation in the associated morbidity, interval between the original event and the development of the hydrocele, and the side of developed hydrocele is a point of inconsistency for identifying the exact cause in the present series. The primary hydrocele that developed during infancy (Pt. 1) might have resulted from a congenital defect of the lumbar lymph pathway.
Regarding the treatment of non-communicating hydrocele, several strategies such as the removal of the sack [12], fenestration [13], internal drainage [14] and sclerotherapy [15] have been reported. All the patients in the present series underwent a subtotal removal of the sack with the aim of reducing the secretory area of the tunica and the drainage of the residual lymph through the inguinal pathway; none of the patients experienced any further recurrences. Because the outer coverings of the testicle and the neighboring tissues possess their lymph pathways that drain to the inguinal nodes (Figure 5), the lymph generated in the testicular system without tunica vaginalis would be drained through this pathway, our strategy seems rational. Postoperative persistent edema on the scrotum in Pt. 1, 4 and 5 suggests that some considerable period is needed to establish the enough lymph pathways to the inguinal nodes.
Figure 5: Difference in lymph pathways between originally internal genital organs (testis, epididymis and tunica vaginalis) and external organs (scrotum and penis). Abbreviations: S, scrotum; P, penis; V, tunica vaginalis; L, paraaortic lymph nodes; I, inguinal lymph nodes; T, left testicular artery.
In conclusions, the complete occlusion of the PPV does not always prevent the recurrence of hydrocele because of alternative pathogenetic mechanisms. The pathological findings of the sack wall in the presently reported cases suggested the impaired drainage of lymph flow in the testicular system. In these cases, the subtotal removal of the sac wall was the treatment of choice. Because of the difficulty in identifying and treating a tiny PPV associated with a hydrocele through an inguinal incision, a direct operative approach to the IIR or the neck of the sac must be avoided to prevent further damage to the lymph drainage system. Consequently, diagnostic laparoscopy is advisable to distinguish between hydroceles that are or are not associated with a PPV.
Acknowledgments
The authors thank Dr. Seiya Akatsuka of Department of Clinical Pathology, Saitama City Hospital and Drs. Rei Kin and Hidekazu Kayano of Department of Central Diagnostic Pathology, Saitama Medical University for their interpretation of histopathological findings and Dr. Ryosuke Satake of Department of Pediatric surgery, Saitama Medical University for his cooperation in preparing this manuscript.
References
- Koop CE. Groin hernia in infants and children. In: Nyhus LM, Condon RE (eds). Hernia, 4th edn. Philadelphia: JB Lippincott. 1995; 109-110.
- Endo M, Watanabe T, Nakano M, Yoshida F, Ukiyama E. Laparoscopic completely extraperitoneal repair of inguinal hernia in children: a single-institute experience with 1,275 repairs compared with cut-down herniorrhaphy. Surg Endosc. 2009; 23: 1706-1712. Ref.: https://goo.gl/2u9SVn
- Endo M, Nakano M, Watanabe T, Ohno M, Yoshida F, et al. Laparoscopy assisted one-stage trans-scrotal orchidopexy applicable to all types of maldescended testes. In: Shamsa A (ed.). Advanced Laparoscopy. Rijeka: InTech. 2011; 55-66. Ref.: https://goo.gl/Ly8Hzy
- Ein SH, Nasr A, Wales P, Gerstle T. The very large recurrent postoperative scrotal hydrocele after pediatric inguinal hernia repair: a rare problem. Pediatr Surg Int. 2009; 25: 239-241. Ref.: https://goo.gl/WFPjTb
- Climador M, Castagnetti M, DeGrazia E. Management of hydrocele in adolescent patients. Nat Rev Urol. 2010; 7: 379-385. Ref.: https://goo.gl/7yCmxR
- Ku JH, Kim ME, Lee NK, Park YH. The excisional, plication and internal drainage techniques: a comparison of the results for idiopathic hydrocele. BJU Int. 2001; 87: 82-84. Ref.: https://goo.gl/RruAKf
- Wilson JM, Aaronson DS, Schrader S, Baskin LS. Hydrocele in the pediatric patient: Inguinal or scrotal approach?. J Urol. 2008; 180: 1724-1728. Ref.: https://goo.gl/T5MoUn
- Wallace AF. Aetiology of the idiopathic hydrocele. Br J Urol. 1960; 32: 79-96. Ref.: https://goo.gl/ZDPXzP
- McBrien MP, Edwards JM, Kinmonth JB. Lymphography of the testis and its adnexa in the normal and in idiopathic hydrocele. Arch Surg. 1972; 104: 820-825. Ref.: https://goo.gl/8Wo5Sc
- Oswald J, Brenner A, Brenner E, Fritsch H, Schlenk B. Pattern of lymphatic drainage of human testes with respect to hydrocele formation after varicocelectomy in adolescents. J Pediatr Urol. 2009; S81. Ref.: https://goo.gl/bvrN3d
- Fourie N, Banieghbal B. Pediatric Hydrocele: A complihensive review. Clin Surg. 2017; 2: 1448. Ref.: https://goo.gl/vYX1g1
- Onol SY, Llbey YO, Onol FF, Ozbek E, Arslan B, et al. A novel pull-through technique for the surgical management of idiopathic hydrocele. J Urol. 2009; 181: 1201-1205. Ref.: https://goo.gl/DkWkvg
- Nigam VK. Window operation: new technique for hydrocele. Urology. 1984; 24: 481-482. Ref.: https://goo.gl/6NLPah
- Aslan M, Kilinc M, Yilmaz K, Ozturk A. A new approach in the management of the hydrocele with a silicone catheter. Urology. 2004; 63: 170-173. Ref.: https://goo.gl/osknVY
- Hu KN, Khan AS, Gonder M. Sclerotherapy with tetracycline solution for hydrocele. Urology. 1984; 24: 572-576. Ref.: https://goo.gl/QY8x4f
- Ozdilek S. The pathogenesis of idiopathic hydrocele and a simple operative technique. J Urol. 1957; 77: 282-284. Ref.: https://goo.gl/85uvE5
- Endo M, Ohno M, Yoshida F, Nakano M, Watanabe T, et al. Laparoscopic hernia repair and its validation by second-look inspection to internal inguinal rings in children with patent processus vaginalis. In: Meinhold-Heerlein I (ed.). Laparoscopy - An Interdisciplinary approach. Rijeka: In Tech. 2011; 133-146. Ref.: https://goo.gl/ce6Guw