Research Article
“Iliosacral bridging” - A new alternative minimal invasive fixation of unstable pelvic ring fractures

Siekmann H1*, Becherer L1, Neef R1, Kunath T1 and Florian Radetzki2
1Martin Luther University Halle-Wittenberg, Department of Orthopedic, Trauma and Reconstructive Surgery, Ernst-Grube-Str. 40, 06120 Halle (Saale), Germany2Dessau Municipal Hospital, Department of Orthopedic and Trauma Surgery, Auenweg 38, 06847 Dessau-Roßlau, Germany
*Address for Correspondence: Dr. Med. Florian Radetzki, Dessau Municipal Hospital, Department of Orthopedic and Trauma Surgery, Auenweg 38, 06847 Dessau-Roßlau, Germany, Tel: 0340 501-3600; Email: florian.radetzki@gmx.de; florian.radetzki@klinikum-dessau.de
Dates: Submitted: 31 October 2018; Approved: 19 November 2018; Published: 20 November 2018
How to cite this article: Siekmann H, Becherer L, Neef R, Kunath T, Radetzki F. “Iliosacral bridging” - A new alternative minimal invasive fixation of unstable pelvic ring fractures. Arch Surg Clin Res. 2018; 2: 039-046. DOI: 10.29328/journal.ascr.1001022
Copyright License: © 2018 Siekmann H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pelvis; Pelvic ring; Osteoporotic fracture; Insufficiency fracture; Classification; Treatment; Osteosynthesis; Iliosacral bridging; Transsacral bar; Iliolumbar fixation; Sacroiliac screw
Abstract
Introduction: Fractures of both the anterior and posterior pelvic ring are common injuries in polytrauma and the elderly that extend beyond those of simple low-impact trauma. While conventional X-rays predominantly show the ventral aspect of the injury, computed tomography often detect additional fractures of the sacrum. A large number of these fractures are B-injuries by AO, mainly compression fractures at an advanced age. In addition, the prevalence of pelvic insufficiency fractures caused by osteoporosis rather than subsequent to an obvious trauma is increasing, with such an injury often associated with pain that impairs mobilization. The standard sacroiliac screw fixation is often characterized by loosening and thus failure of the osteosynthesis especially in osteoporotic bone of elderly patients.
Method: A new alternative surgical minimal invasive technique, the “iliosacral bridging”, stabilizes the fractures of the sacrum with an internal fixation from S1 pedicle of the uninjured side to the ilium on the affected side. The combination of this internal fixation with the standard single sacroiliac screw on the injured side allows an immediate full weight bearing and pain free mobilization. We present a case series of 8 patients.
Results: The clinical and radiological analysis analogous to the pelvic-outcome-score brought forward that 2 patients showed an excellent and 2 patient a good result. The other 4 patients achieved sufficient results.
Conclusions: The “iliosacral bridging” we have introduced in the present study provides evidence of an expected increased stability of the pelvis after B-injuries
Introduction
Fractures of the pelvic ring classified as lower severity with the exception of vertical unstable pelvis C-fractures had previously been the domain of the nonsurgical therapy until 20 -25 years ago [1]. While young patients were mainly affected by such injuries in the context of polytrauma, nowadays (at least according to the demographic development) elderly patients are more often affected within the context of a single trauma after inadequate accidents as well as a cause of insufficiency fractures without any trauma [2-4]. With an increasing knowledge of the morphology of fractures caused by the introduction of computed tomography, but also from the perspective of a better kind of mobilization of patients, diverse procedures of therapy have increasingly found entrance into the treatment of these injuries. In addition to simple dorsal osteosythesis with screws dorsoventral procedures are also applicable as well as, especially with elderly patients the application of bonecements for the purpose of sacroplasty and also within the cement augmentation of the used implants. The different risks and complications that are combined with these procedures have to be considered. The complex anatomy and diversity of shape of the posterior pelvic ring have a big influence on this. The sacroiliacal screw fixation with one screw still involves a high rate of loosening of the implants. The use of two screws is more complicated for the surgeon, with the risk of dislocated screws increasing. If there is a presence of a so-called sacrum dysplasia, it is rarely or not possible to insert an SI-screw, while the use of cement (sacroplasty, screw augmentation) over the last years has been shown to cause cement extravasation as well as (cement) embolism. In the present article, therefore, we introduce an alternative method to stabilize the horizontally unstable fractures of the pelvis. Based on numerous clinical cases and contemporary literature, we will attempt to summarize the advantages and limitations of this alternative approach.
Method
By the end of 2010, our clinic had performed the isolated dorsal “iliosacral bridging” of the posterior pelvic ring, treating 11 patients (25-88 years old) that suffered fractures of the pelvic ring type B by AO. Cause of incident ranged from high energy trauma (e.g., following management of polytrauma) to a low energy single trauma (e.g, caused by a domestic fall). These fractures are cases of pelvis B-fractures type B2.1 or type B2.2 by AO [13], as well as transalare (zone1) or transforaminale (zone2) fractures of the sacrum by Denis [11]. All patients had sustained the fracture from a trauma, whereas no patient had an insufficiency fracture.
Surgical technique
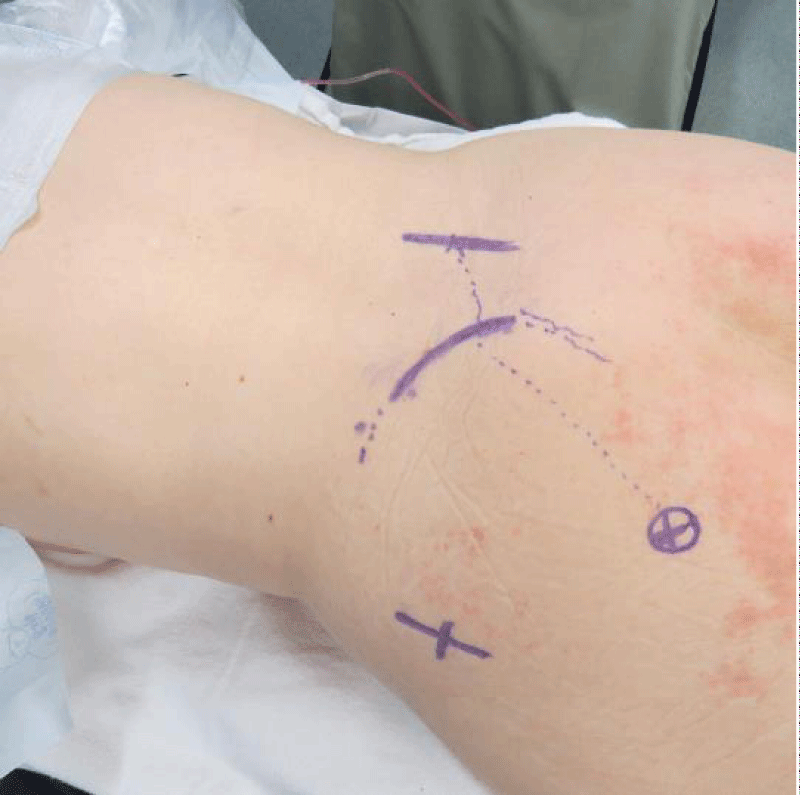
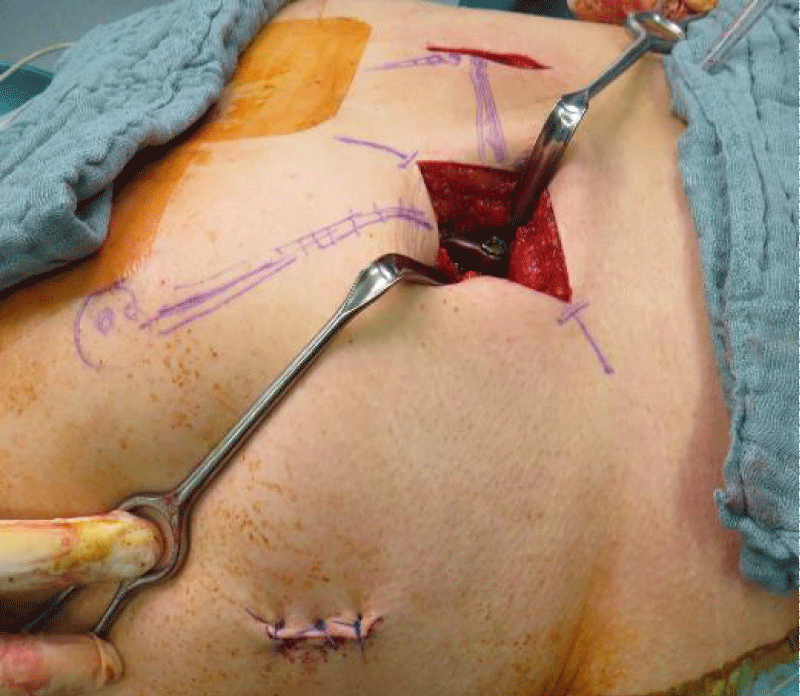
Common prone position: Checking presentability throughout the usual planes under image converter. In the process, local anatomy (dorsal iliac ala, iliosacral joint and centre of femoral head on the injured side, pedicel SWK 1 on the healthy side) are marked (Figure 1) as well as the accesses (just lateral and kranial iliosacral joint and incision for the transiliosacral screw on the injured side, axial marking discreetly lateral of SWK 1-pedical on the healthy side). Starting with the transiliosacral screw, which has always been used so far as a fully threaded screw with washer (diameter 7,3 mm) in established cannulated technique. Attention regarding screw length, which must not irritate the subsequent placement of the polyaxial screw in pedicel S1 on the healthy side. The length of the screw is usually approximately 80-100mm. Now placement of the 1st polyaxial screw on the dorsal iliac crest of the injured side. For this purpose an approximately 5-7cm long slightly oblique incision is placed around 1 cm cranial and parallel to the Crista iliaca. The fascia is cut off sharply straight above its attachment at the iliac crest. Because the polyaxial screws under the soft tissue on the iliac crest can dorsally be prominent, it is necessary to prepare with the Luer a groove of approximately 1.5 x 1.5 x 1.0cm. The screw may be placed at the inner side of the iliac crest in order to reduce the extent of soft tissue exposure. From here the preparation of screw deposit by use of a blunt awl is done towards the center of the femoral head. Especially within the osteoporotical bone, the cancellous bone is easy to feel with the help of the awl and therefore the proper preparation generally perceptible. Basically the position of the screw is controlled on all sides by the palpation probe after preparation. In the case of unclear findings, then to control the position an intraoperative fluoroscopy tangential to the Ala ossis ilium, can be performed while the awl or palpation probe are in place. Placement of the 2nd polyaxial screw (usually 100-120mm) in the position described by Schildhauer [31,32]. Longitudinal incision and preparation above the pedicel SWK1 on the healthy side: Preparation of the screw position with the help of a sharp and blunt awl, whereas the 2nd sacral cortex is perforated in order to get a better fixation. Open the pedicle using a pedicle probe. Screws of 40-50mm length according to the anatomy are used [33]. Tunneling of the muscles between the inserted screws: Assembling of the slightly curved rods via connector and wound closure (Figure 2).
Figure 1: Local anatomy (dorsal iliac ala, iliosacral joint and centre of femoral head on the injured side, pedicel SWK 1 on the healthy side) are marked as well as the accesses.
Figure 2: By the end of the surgery tunneling of the muscles between the inserted screws: Assembling of the slightly curved rods via connector and wound closure.
Postoperative care
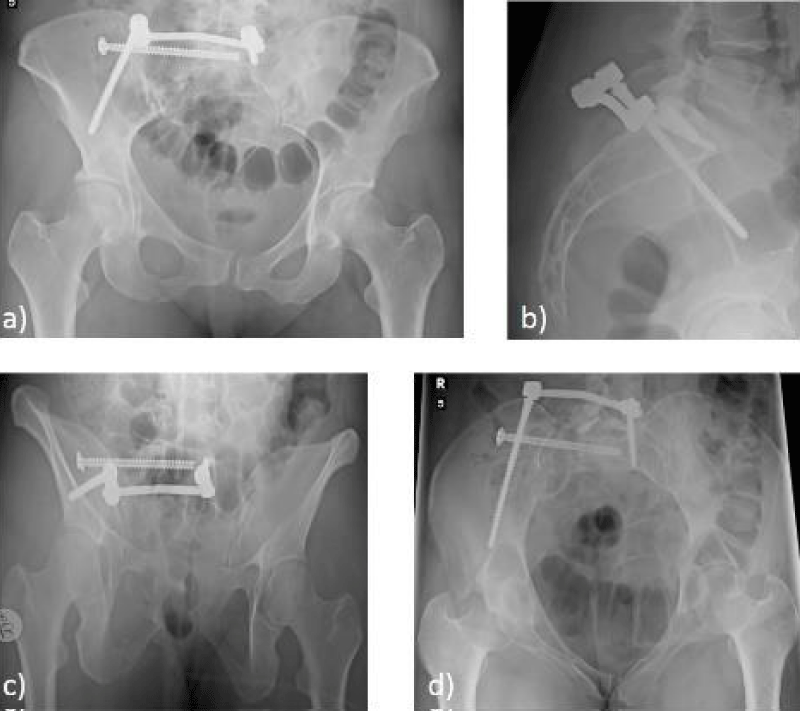
Up until this point, the mobilization of patients took place under professional physiotherapy with immediate full weight bearing which included the injured side. Prophylaxis against thrombosis as well as analgesia. Radiological control after 1 day and 2+6 weeks postoperative (Figures 3a-d). Removal of material only in younger patients.
Figure 3: Radiological control shows the result of the stabilization in a) a.p., b) lateral, c) outlet and d) inlet view.
In order to analyze outcomes and recognize the extent of clinical symptoms as well as evaluating social factors, a detailed examination of the body took place and standardized questionnaires were applied. Corresponding symptoms of pain of the distal lumbar spine and the pelvis were found, functional impairments, neurological-sensomotorical deficits and additional urological and sexual dysfunction (pre- and postoperative). In addition restrictions in profession, sport and leisure activities as well as social reintegration after the operative treatment were documented. Implementation of x-ray then was performed during follow-up making an a.p.–radiograph of the pelvis as well as inlet and outlet images of the pelvis. The diagnosis was done by an independent investigator with the focus on dislocation of the posterior pelvis as well as dislocation of the ischiopubic bone and also of the anterior pelvis ring. The gained results were validated against the pelvis-outcome-scores.
Results
Between 01.07.2014 to 31.07.2016, 12 patients with a pelvis-B-injury classified by AO were treated operatively through monolateral transiliosacral bridging. For a recall study the rate of return was 66,7%. There with the definite collection of patients was 4 masculine and 4 feminine with an age ranging from 25 up to 77 years, having an average age of 51,9 years.
Causes of injury were high-speed and single traumas in 62,5% and 37,5%, respectivley. The average follow-up was 9,9 months. The pelvis fractures were classified by AO standards. With 7 patients it was a 61-B2.1b2c1 and with 1 patient it was a 61-B2.1b1c3 fracture (Table 1).
| Table 1: Meta-data of 8 patients treated with monolateral iliosacral bridging. | |
| patients, n (%) | |
| age (years) mean range |
51.9 25-77 |
| follow-up (months) mean range |
9,6 8-13 |
| sex female male |
4 (50,0) 4 (50,0) |
| type of injury monotrauma polytrauma |
3 (37,5) 5 (62,5) |
| type of fracture 61-B2.1b2c1 61-B2.1b1c3 |
7 (87,5) 1 (12,5) |
Five patients stated at follow up subsequent no symptoms of pain, while 3 of them complained about pain under light stress. None of them complained about permanent pain in the area of the pelvis and the lumbar spine. Functional deficits were not determined in 4 patients, 2 patients stated light impairments, 1 patient stated marked impairments. Permanent disorders were not discriminated in any patient. Two of them stated light deficits of sensibility in the area of N. cutaneus femoralis lateralis, for 1 female patient was verified a restriction of the active flexion of the right hip joint (power level 4 of 5 by Janda) which had been already present right after the trauma. The same patient complained also about sexual disorder since the operative treatment. In addition, another female patient complained about slight urological deficits, which was a pre-existing problem.
Radiological examination
With 7 patients the anatomic healing or only minor malposition of the anterior pelvis ring <5mm or of the ischiopubic bone <10mm is registered. One female patient had a bigger malposition of the anterior pelvis ring, although under 10 mm.
Social reintegration
Six patients recovered without any restrictions post-operation and have returned to their professional life, 2 stated slight restrictions. Five patients were enabled to get back to their former sports and leisure activities, 3 patients have a restricted level of activity, none was obvious restricted or not active at all. The social situation was steady in 7 patients, with 1 patient stated a slight restriction of social activity. All patients denied dependence of external help.
The interpretation of the clinical and radiological analysis analogous to the pelvic-outcome-score brought forward that 2 patients showed an excellent and 2 patient a good result. The other 4 patients achieved sufficient results (Table 2).
| Table 2: Pelvic-Outcome-Score and social reintegration of 8 patients after surgical treatment with monolateral iliiosacral bridging and follow-up. | ||||
| Patient | Pelvic-Outcome (points) | Social reintegration (points) | ||
| Clinical | Radiological | Total | ||
| 1 | 4 | 3 | 7 | 3 |
| 2 | 3 | 3 | 6 | 3 |
| 3 | 2 | 3 | 5 | 2 |
| 4 | 2 | 3 | 5 | 3 |
| 5 | 2 | 3 | 5 | 3 |
| 6 | 2 | 2 | 4 | 2 |
| 7 | 4 | 3 | 7 | 3 |
| 8 | 3 | 3 | 6 | 2 |
| Score-results Pelvic-Outcome (points): excellent (7) good (6) adequate (4-5) inadequate (1-3) Score-results social reintegration (points): unchanged (3) restricted (2) disabled (1). |
||||
Discussion
The essential aim of the therapy of pelvis ring injuries type B by AO is to be able to provide adequate mobilization of patients under analgesics adapted to full weight bearing. This response plays a decisive role in avoiding secondary complications (pressure ulcers, thrombosis, embolisms, pneumonia), particularly in the elderly. Only when conservative therapeutic methods combination with administration of analgesics and physiotherapies fail, operative therapy is recommended [14-16]. Regular radiological monitoring is also an important factor [17].
Primarily the transiliosacral screw fixation is a relatively simple manageable operative procedure. The common complications of an operation are seen next to the risk of relevant neurological lesions. Additional problems of the procedure are loosening of the implants as a matter of missing rotation stability of the osteosythesis. To increase rotation stability, a double iliosacral screw fixation is postulated [18,21,23]. In this particular case two screws can be inserted into the small implantation corridor parallel or diagonally converging in the SWK 1 or approximated parallel in SWK 1 and SWK 2. The risks for placing screws in the incorrect positions with implantation of two screws are significantly higher. As in operations of the spine also with the screw fixation of sacrum fractures the augmentation of the screw deposit by techniques of cementing can be used [24,25]. Besides the risks and complications that are resting on the prementioned techniques of operations, the problems also are extravasation and embolism caused by cement. Furthermore the cement generally cannot be removed in the case of an infection.
After a successful introduction of kyphoplasty within the spine surgery, the realization of technique was followed also with fractures of the sacrum called sacroplasty. A partly obvious reduction of pain is described by several authors [19,26-28]. Since the used cements however are often not adequate for the local shear forces, the achievement of stabilization of the fracture is at least doubtful. Also with this method, the question next to the common operation risks are how it is going to be dealt with the applied cement in case of infection or cement extravasation [29].
With the so called “open-book”-injuries exclusively isolated ventral techniques are broadly practiced. With dorsoventral osseous injuries or dorsal fragmentations of the Os sacrum can be done an additional ventral stabilization of the anterior pelvis ring (usually pubis bone) by the use of a plate or percutaneous by use of a lokal “creeping screw” besides the dorsal stabilization of the sacrum fracture e.g. through a sacroiliac joint screw in order to increase stability. Based on an additional operative access, the risk for corresponding complications including required change of the patient’s position and the time of operation are increased.
From our perspective, the following advantages emerge out of our introduced procedure: “iliosacral bridging” reaches also rotation stability as well as the usage of two SI-screws. Against the horizontal implantation of these two screws our screw is lying distinctly further away from the additional longitudinal support, with the result that both the rotation lever and horizontal powers of lever can be neutralized obviously stronger. This applies even more obviously when both SI-screws one above the other are converging in SWK 1 or are arranged in SWK 1 and 2 parallel vertical one above the other and here in the case of horizontal forces rather function like a door hinge. The horizontal assembly of the rod behind the screw SWK 1 is also possible with sacrum dysplasia. As well as the implantation of iliosacral (SI-) screws, the implantation of osteosythesis materials within the “iliosacral bridging” is minimally invasive. Also without the use of increased cements, the mobilization of patients under full stress/weight bearing was possible. In our opinion this is due to the horizontal positioning of the implanted materials but also the screw fixations that obviously higher the total length of the fixing screws (approx. 90 vs. 180 vs. 260 mm) concerning the young as well as the elderly patients which were operated in the described way. Supplementary ventral stabilizations were not necessary yet.
That way the “iliosacral bridging” with a still minimal invasive operation technique including slightly bigger accesses gives reason to expect a significant increase of stability. An intraoperative change of position, which is partly necessary within the dorsoventral procedure, is excluded.
A control of the osteosynthesis via a finite elements model as well as a biomechanical cadaveric study to control stability of described osteosynthesis are in progress.
Conclusion
The “iliosacral bridging” we have introduced in the present study provides evidence of an expected increased stability of the pelvis after B-injuries. One potential explanation may be related to the horizontal assembly of the osteosynthesis (transiliosacral screw and iliosacral dorsal internal fixation rod), which acts better against the injury associated flexural forces than the vertical ordered screws. In addition, the obviously higher total length of the fixing screws compared to isolated transiliosacral screws to obtain a higher stability may also contribute. The described osteosynthesis also allowed an adapted full weight bearing response, with no required change of the patient’s position during the operation as well as minimal invasive incisions. The evidence level of the study is IV.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
References
- Gilliland MD, Ward RE, Barton RM, Miller PW, Duke JH. Factors affecting mortality in pelvic fractures. J Trauma 1982; 22: 691-693. Ref.: https://goo.gl/MkAo1t
- Keller JM, Sciadini MF, Sinclair E, O'Toole RV. Geriatric trauma demographics, injuries, and mortality. J Orthop Trauma. 2012; 26: e161-e165. Ref.: https://goo.gl/2tmKuj
- Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury. 2013; 44: 1733-1744. Ref.: https://goo.gl/6Jo4xn
- Sullivan MP, Baldwin KD, Donegan DJ, Mehta S, Ahn J. Geriatric fractures about the hip: divergent patterns in the proximal femur, acetabulum, and pelvis. Orthopedics. 2014; 37: 151-157. Ref.: https://goo.gl/27u3TS
- Frick H, Leonhardt H, Starck D. Taschenlehrbuch der gesamten Anatomie I. Allgemeine Anatomie. Spezielle Anatomie I. Extremitäten, Rumpfwand, Kopf, Hals. Mit Schlüssel zum Gegenstandskatalog. 4. Auflage ed. Stuttgart: Thieme 1992;
- Galbraith JG, Butler JS, Blake SP, Kelleher G. Sacral insufficiency fractures: an easily overlooked cause of back pain in the ED. Am J Emerg Med 2011; 29: 359-356. Ref.: https://goo.gl/95dD72
- White JH, Hague C, Nicolaou S, Gee R, Marchinkow LO, et al. Imaging of sacral fractures. Clin Radiol 2003; 58: 914-921. Ref.: https://goo.gl/EXMwzq
- Cabarrus MC, Ambekar A, Lu Y, Link TM. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol. 2008; 191: 995-1001. Ref.: https://goo.gl/iNyzzz
- Ahovuo JA, Kiuru MJ, Visuri T. Fatigue stress fractures of the sacrum: diagnosis with MR imaging. Eur Radiol. 2004; 14: 500-505. Ref.: https://goo.gl/j3WRZK
- Pohlemann T, Gansslen A, Tscherne H. [Fracture of the sacrum]. Unfallchirurg. 2000; 103: 769-786.
- Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988; 227: 67-81. Ref.: https://goo.gl/oFzSa6
- Koo H, Leveridge M, Thompson C, Zdero R, Bhandari M, et al. Interobserver reliability of the young-burgess and tile classification systems for fractures of the pelvic ring. J Orthop Trauma. 2008; 22: 379-384. Ref.: https://goo.gl/FdTrAh
- Tile M. Fractures of the pelvis and acetabulum. 2nd ed. Baltimore: Williams & Wilkins. 1995;
- Giannoudis PV, Tzioupis CC, Pape HC, Roberts CS. Percutaneous fixation of the pelvic ring: an update. J Bone Joint Surg Br. 2007; 89: 145-154. Ref.: https://goo.gl/ugZ9fC
- Grubor P, Milicevic S, Biscevic M, Tanjga R. Selection of treatment method for pelvic ring fractures. Med Arh. 2011; 65: 278-282. Ref.: https://goo.gl/fg9Fpp
- Mendel T, Noser H, Wohlrab D, Stock K, Radetzki F. The lateral sacral triangle--a decision support for secure transverse sacroiliac screw insertion. Injury. 2011; 42: 1164-1170. Ref.: https://goo.gl/BYkYk2
- Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil. 2002; 79: 404-409. Ref.: https://goo.gl/5BaEo9
- Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989; (242): 83-97. Ref.: https://goo.gl/pyS5f9
- Mears SC, Sutter EG, Wall SJ, Rose DM, Belkoff SM. Biomechanical comparison of three methods of sacral fracture fixation in osteoporotic bone. Spine (Phila Pa 1976) 2010; 35: E392-E395. Ref.: https://goo.gl/BL36ZJ
- Routt ML, Jr., Simonian PT, Agnew SG, Mann FA. Radiographic recognition of the sacral alar slope for optimal placement of iliosacral screws: a cadaveric and clinical study. J Orthop Trauma. 1996; 10: 171-177. Ref.: https://goo.gl/yE2LAc
- Carlson DA, Scheid DK, Maar DC, Baele JR, Kaehr DM. Safe placement of S1 and S2 iliosacral screws: the "vestibule" concept. J Orthop Trauma. 2000; 14: 264-269. Ref.: https://goo.gl/rfuBAW
- Tosounidis T, Kanakaris N, Nikolaou V, Tan B, Giannoudis PV. Assessment of Lateral Compression type 1 pelvic ring injuries by intraoperative manipulation: which fracture pattern is unstable? Int Orthop. 2012; 36: 2553-2558. Ref.: https://goo.gl/YUACk3
- van Zwienen CM, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma. 2004; 18: 589-595. Ref.: https://goo.gl/uFxqzv
- Wahnert D, Raschke MJ, Fuchs T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum: a new method using modified implants. Int Orthop. 2013; 37: 1147-1150. Ref.: https://goo.gl/huSi7G
- Yu BS, Yang ZK, Li ZM, Zeng LW, Wang LB, et al. Which is the preferred revision technique for loosened iliac screw? A novel technique of boring cement injection from the outer cortical shell. J Spinal Disord Tech. 2011; 24: E49-E56. Ref.: https://goo.gl/LLbNyp
- Frey ME, DePalma MJ, Cifu DX, Bhagia SM, Carne W, et al. Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J. 2008; 28: 367-373. Ref.: https://goo.gl/3nKGW6
- Shah RV. Sacral kyphoplasty for the treatment of painful sacral insufficiency fractures and metastases. Spine J. 2012; 12: 113-120. Ref.: https://goo.gl/Jv47Pq
- Trouvin AP, Alcaix D, Somon T, Zarnitsky C. Analgesic effect of sacroplasty in osteoporotic sacral fractures: a study of six cases. Joint Bone Spine. 2012; 79: 500-503. Ref.: https://goo.gl/HvHbBp
- Bastian JD, Keel MJ, Heini PF, Seidel U, Benneker LM. Complications related to cement leakage in sacroplasty. Acta Orthop Belg. 2012; 78:100-105. Ref.: https://goo.gl/PyCKdW
- Pohlemann T, Weigel B, Maghsudi M. Praxisbuch Unfallchirurgie. 2nd ed. Berlin, Heidelberg, NY: Springer. 2011;
- Schildhauer TA, Josten C, Muhr G. riangular osteosynthesis of vertically unstable sacrum fractures: a new concept allowing early weight-bearing. J Orthop Trauma.1998; 12: 307-314. Ref.: https://goo.gl/V7LZw9
- Schildhauer TA, McCulloch P, Chapman JR, Mann FA. Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech. 2002; 15: 199-205. Ref.: https://goo.gl/wx7gXb
- Ebraheim NA, Lin D, Xu R, Stanescu S, Yeasting RA. Computed tomographic evaluation of the internal structure of the lateral sacral mass in the upper sacra. Orthopedics.1999; 22: 1137-1140. Ref.: https://goo.gl/vof6rG