More Information
Submitted: 26 August 2019 | Approved: 05 September 2019 | Published: 06 September 2019
How to cite this article: Mansour S, Khouri S, Andraous M, Khuri S. Extremely large hemangioma of the liver: Safety of the expectant management. Arch Surg Clin Res. 2019; 3: 061-064.
DOI: 10.29328/journal.ascr.1001036
Copyright License: © 2019 Mansour S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Extremely large hepatic hemangioma; Conservative management
Extremely large hemangioma of the liver: Safety of the expectant management
Subhi Mansour1, Sharbel Khouri2, Maisa Andraous3 and Safi Khuri1,4*
1Department of General Surgery, Rambam Health Care Campus, Haifa, Israel
2Department of Radiology, Galilee Medical Center, Nahareya, Israel
3Department of Radiology, Rambam Health Care Campus, Haifa, Israel
4HPB and Surgical Oncology Unit, Rambam Health Care Campus, Haifa, Israel
*Address for Correspondence: Safi Khuri, Department of Surgery, HPB and Surgical Oncology Unit, Rambam Health Care Campus, Haifa, Israel, Tel: 00972502062169; Email: [email protected]
Hemangiomas are known as congenital vascular malformations that can affect almost any organ or tissue, with the liver being the most common intra-abdominal organ to be involved. It is well known that hemangiomas are the most common benign tumours of the liver, and develop in about 4-20% of people, mainly young adult females. Recently, due to the dramatic rise in the use of imaging studies for different purposes, a parallel increase in the incidence of these tumours has been noticed. Most liver hemangiomas are small (less than 4cm in diameter), asymptomatic and found incidentally during abdominal operation for other indication or on radiologic studies. Giant liver hemangioma is defined as hemangioma with a diameter of more than 5cm. This unique and uncommon type of haemangioma usually poses therapeutic challenges for the treating physician, especially hepatic surgeons, due to the unclear natural history, and due to the risk of life threatening complications is yet to be established. While it is already proved by several studies that conservative management of giant hepatic hemangioma is safe, it is not known whether observation of the extremely large hepatic hemangioma (tumours larger than 10cm) is safe as well.
The aim of this article is to review the English literature to find out if conservative management of the extremely giant liver hemangioma is safe and can be recommended.
Hemangiomas are well known congenital vascular malformations, and sometimes are referred to as cavernous hemangiomas or cavernomas. Although genetic predisposition has been proposed, the exact aetiology for this tumour is still unknown. These lesions can affect any organ site of the body, with the scalp and face being the most commonly affected sites [1]. Hemagiomas, a benign tumour that enlarge by ectasia rather than hypertrophy or hyperplasia, can vary in size from few millimetres to several centimetres in diameter [2]. The current evidence indicates that these tumours have no malignant potential. Intraabdominally, hemangioma can develop anywhere, such as solid organs, ligaments, hollow viscera or in the abdominal wall, with the liver being the most common abdominal organ to be involved [1]. Of all tumours affecting the liver, hemangioma is the second most common following metastasis and the most common benign mesenchymal tumour. Although its precise incidence is unknown, it is estimated to affect about 4-20% of the general population [3]. Recently, due to the dramatic increase in the number of people undergoing different radiologic imaging techniques, a parallel rise in the incidence of this tumour has been noticed [4]. Hepatic hemangiomas can affect any age group, with young adult females being the most common group to have this tumour (F:M ratio 5:1) [5]. Most of the tumours are detected between the third and the fifth decade of life. Macroscopically, these tumours are hypervascular, well- circumscribed lesions; while microscopically, they are described as variably sized vascular spaces lined by flat endothelial cells, filled with ectatic blood and separated by fibrous septa. Different types of hepatic hemangiomas were reported, with the cavernous subtype being the most common and constitute about 80%, while the papillary subtype is less common and is characterized by being usually smaller with multiple growths. Giant hemangioma has always been defined as tumour larger than 5cm diameter, but recently, new classification for these tumours according to size has been advocated; Small hemangiomas are tumours with a diameter of 1-2cm, typical hemangiomas are 2cm-10 cm in diameter and giant hemangiomas are larger than 10cm [6,7]. Most physicians still define giant liver hemangioma as a lesions larger than 5cm.
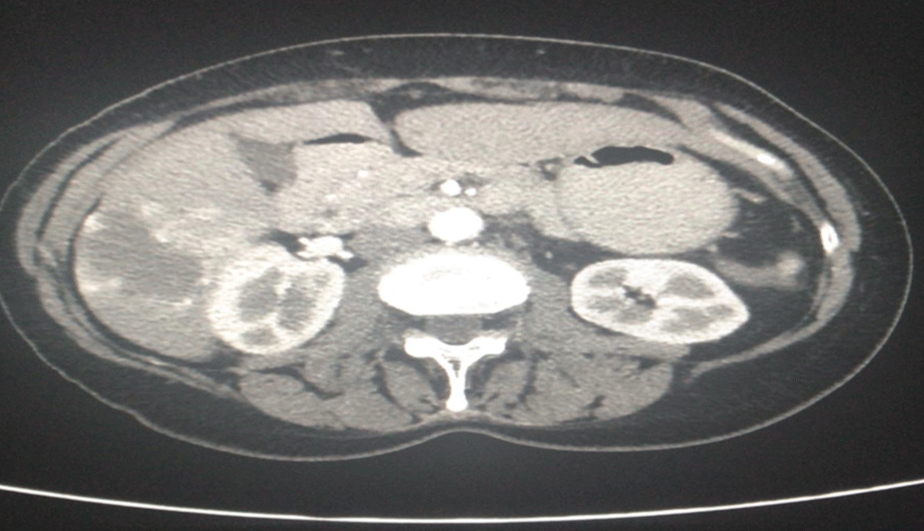
Most hepatic hemangiomas are small (less than 4cm in diameter) and asymptomatic, and diagnosed incidentally either by imaging studies or during abdominal operations done for other surgical indications (Figure 1). For the majority of people who are known to have liver hemangioma, the natural history remains uneventful, with observations by means of regular follow ups and radiologic studies being adequate [8,9]. While almost all small asymptomatic hemangiomas are safely observed, the unclear natural history and the possibility of future complications for giant haemangioma, especially tumours larger than 10cm in diameter, makes management of this specific type of tumour a controversial issue for the treating physician [10]. Indications for surgical interventions include diagnostic uncertainty, spontaneous or traumatic rupture, rapid lesion growth, consumptive coagulopathy (Kasabach-Merrit syndrome) and severe symptoms - mainly severe abdominal pain due to giant lesions causing stretching of the Glisson capsule of the liver [11-13].
Figure 1: An axial abdominopelvic Computed Tomography (CT) scan demonstrates an incidental finding of giant hepatic hemangioma at the right lobe of the liver. CT scan was done due to suspicion of diverticulitis of the sigmoid colon.
Objective
The review article was performed to explore the different relevant studies in the English literature to figure out if conservative management of the extremely giant liver haemangiomas, larger than 10cm, by wait and see strategy is safe and can be routinely recommended.
A search of studies was conducted on PubMed. A term strategy based on PICOS acronym was adopted, using subjects heading and text words that allow to identify studies including patients with extremely large hepatic haemangioma (larger than 10cm), who were assigned for conservative vs. non-conservative treatment.
The following search strategy was used on the PubMed database including the following search terms: “hepatic haemangioma” “haemangioma of the liver”, “giant liver haemangioma”, “conservative management of giant hepatic haemangioma”, giant haemangioma of the liver: conservative vs. surgical management”.
Reviewing the current English literature reveals countless studies, mainly retrospective and limited to single center experience, who approved that expectant management for the typical hepatic hemangioma is safe. The primary outcomes assigned in these studies differ based on the purpose of the study in question, the key outcomes discussed are the development of new symptoms and the incidence of complications. The risk of complications during observation of this specific type of tumor is low and stands at less than 20%. The risk for life threatening complications, such as spontaneous rupture, is extremely low at about 2%. Nevertheless, studies regarding the safety of expectant management of the extremely large hepatic hemangioma (larger than 10cm), are lacking. Patients with this precise hepatic pathology were usually included as part of patients with giant liver hemangioma (larger than 5cm). Thus, Data regarding management of the extremely large hepatic hemangiomas is subpar at best.
While some surgeons believe that extremely large hemangiomas have greater potential for rupture, growth or internal bleeding, and thus, prophylactic resection should be offered; In other author’s experience, size alone should be regarded as a poor predictor for future behavior of extremely large hepatic hemangiomas and should not be considered as an absolute indication.
The following is a review of the relevant studies. Upon conducting the aforementioned search algorithm seven studies reporting patients with extremely large hepatic hemangioma were found, these patients were part of a larger group of patients with giant hemangiomas. Out of these 7 studies, one study did not specify the different size of giant hemangioma, but nonetheless included due to its high number of patients.
All patients, 18 years or older, with hepatic hemangioma of 10cm or larger were included. Articles examining hemangiomas smaller than 10cm were excluded.
Studies were categorized into two groups; Supportive and opposed to the expectant management for the extremely large hepatic hemangiomas (larger than 10cm).
Studies supporting expectant management
Schnelldorfer reported a retrospective study over 20 years, including 289 patients with giant liver hemangiomas [14]. 233 patients were treated conservatively. 42 out of 233 (18%) had extremely large hemangiomas (more than 10cm). The frequency of new onset of symptoms, such as chronic abdominal pain, and overall complications for patients with extremely large hemangiomas were not significantly greater than patients with hemangiomas smaller than 10cm (14% vs. 7%) on a median follow up period of 11 years.
Moreover, a study conducted by Yedibela [15], which included 246 patients, demonstrated that only 9% of patients in the conservative management group developed complications, with two fatal cases reported due to traumatic rupture of the hepatic hemangioma. In this specific study, sizes of hemangiomas were not reported and no correlation between size and complications were conducted.
Herman, et al. [16] published an article summarizing 14 year of experience managing hepatic hemangiomas. 249 patients were included, with 16 patients (6.4%) having hepatic hemangioma larger than 10cm in diameter. This group of patients suffered refractory pain more frequently than the group with the lower scaled hemangiomas. 8 patients (all with tumor size more than 14cm) out of 16 patients, underwent surgery (lobectomy or segmentectomy) mostly due to untreatable pain and all patients were free of pain on follow up. The other 8 patients with hemangiomas larger than 10cm were observed and did not develop any complications or new symptoms.
The results of the previous studies support the expectant management for the extremely large liver hemangioma.
Studies opposed to expectant management
On the contrary, Erdogan, et al. [12] reported a retrospective study including 34 patients with liver hemangioma, of which 14 patients underwent resection. The mean size of the tumor for patients who underwent surgery was 10.3cm and the indication for surgery was upper abdominal pain in most patients (11/14). Only one patient had persistent abdominal pain following the resection of an 8 cm liver hemangioma. The findings of this study reflect that extremely large hemangiomas (larger than 10cm) are usually symptomatic and are advised to be treated by means of surgery.
Donati, et al. [17] published a review article concerning the risk for spontaneous rupture of liver hemangioma. 97 patients were described, of which 46 (47.4%), mainly elderly patients (older than 40) with comorbidities suffered spontaneous rupture, and 52.6% suffered non spontaneous rupture, which was significantly more common in younger patients. The mean size of the ruptured tumor was 11.2cm, and the overall mortality rate was 35%. The authors concluded that preventive surgery should be considered for lesions of at least 11-cm in size.
In his study, Giuliante [18] reported the approach for liver hemangioma in a single center with 74 patients included. 40 patients (out of 74) underwent surgical management due to different indications such as abdominal pain, uncertain diagnosis, Kasabach-Merrit syndrome and tumor enlargement. It is worth mentioning that the average tumor size for the operated group was 11.9cm vs. 6cm in the conservative group. Again, Giuliante study supports the assumption that hepatic hemangiomas larger than 10cm are indicated to be treated surgically due to several impending symptoms and complications.
Another study that builds on the same merit is the study by Zhang, et al. [19] which includes 86 patients with extremely large hepatic hemangiomas. 18 patients (21%) were asymptomatic and incidentally discovered. These patients underwent prophylactic surgical resection due to different indications, including concern of future fatal complications (such as rupture) and due to patient’s preference. Patients were not offered the opportunity of watchful waiting.
Over the last several decades, a dramatic shift in the treatment of giant hepatic hemangioma has occurred, and it is mainly due to multiple studies published. The majority of these studies have approved that expectant management is safe and should be regarded as the gold standard treatment, moreover so in asymptomatic patients and in the absence of other indications for surgical management. Even in the presence of symptoms, which usually include upper abdominal pain or discomfort, a non-related pathology (such as peptic ulcer disease or cholelithiasis) should be excluded before attributing the symptoms to the liver hemangioma [20]. While the mainstay management for giant hepatic hemangioma is clear, the treatment of the extremely large liver hemangioma (larger than 10cm) is not well defined and is regarded as a gray zone for several hepatic surgeons. None of the reported studies have examined the safety of expectant management for the extremely large hepatic hemangiomas. Furthermore, the definition of giant hepatic hemangioma in the English literature consists of a wide array of tumor sizes comprising a range of 5 to 30cm in tumor diameter. Thus, accumulating to the perplexity pertaining to the gold standard management of the extremely large hepatic hemangioma.
Whether or not the expectant management of extremely large hemangiomas of the liver is innocuous remains a debated topic, and surgeons are divided in their opinion regarding this subject, as has been mentioned previously.
This article review introduces conflicting data regarding the management of this precise type of tumor. Thus, treatment of these lesions should be patient specific depending on several factors (medical background, underlying chronic liver disease, presence of other underlying pathology), taking into consideration the associated symptoms and the risk of future complications, particularly rupture of the hemangioma, which has a high mortality rate of up to 35% [17].
In conclusion, as the authors have tried to demonstrate in this review, granted the expectant management of giant hepatic hemangioma is previously evidenced as safe, data regarding the treatment of extremely large hemangiomas of the liver (larger than 10cm) is lacking, and current papers discussing this topic are conflicting in their conclusions. Due to the higher probability of associated symptoms and indications for operation, a tumor scale higher than 10cm should be regarded as a relative indication for surgical or non-surgical intervention (such as angiography), precisely in such cases where the remaining pathologies that may explain the symptoms have been excluded.
- Maestroni U, Dinale F, Frattini A, Cortellini P. Ureteral hemangioma: A clinical case report. Acta Biomed. 2005; 76: 115-117. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16350557
- Tait N, Richardson AJ, Muguti G, Little JM. Hepatic cavernous haemangioma: A 10 year review. Aust N Z J Surg. 1992; 62: 521-524. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1610320
- Choi BY, Nguyen MH. The diagnosis and management of benign hepatic tumors. J Clin Gastroenterol. 2005; 39: 401-412. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15815209
- Lise M, Feltrin G, Da Pian PP, Miotto D, Pilati PL, et al. Giant cavernous hemangioma: diagnosis and surgical strategies. World J Surg. 1992; 16: 516-20. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1589990
- Bioulac-Sage P, Laumonier H, Laurent C, Blanc JF, Balabaud C. Benign and malignant vascular tumors of the liver in adults. Semin Liver Dis. 2008; 28: 302-314. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18814083
- Ketchum WA, Lin-Hurtubise KM, Ochmanek E, Ishihara K, Rice RD. Management of Symptomatic Hepatic "Mega" Hemangioma. Hawaii J Med Public Health. 2019; 78: 128-131. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30972235
- Zhuang BW, Li W, Chen ZF, Cao CJ, Xie XY, et al. Multiple cavernous hemangiomas of the lung and liver mimicking metastasis: A case report and literature review. Medicine (Baltimore). 2018; 97: e13509. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30572451
- Farges O, Daradkeh S, Bismuth H. Cavernous hemangiomas of the liver: are there any indications for resection? World J Surg. 1995; 19: 19-24. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7740805
- Okano H, Shiraki K, Inoue H, Ito T, Yamanaka T, et al. Natural course of cavernous hepatic hemangioma. Oncol Rep. 2001; 8: 411-414. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11182065
- Pietrabissa A, Giulianotti P, Campatelli A, Di Candio G, Farina F, et al. Management and follow-up of 78 giant haemangiomas of the liver. Br J Surg. 1996; 83: 915-918. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8813773
- Yoon SS, Charny CK, Fong Y, Jarnagin WR, Schwartz LH, et al. Diagnosis, management, and outcomes of 115 patients with hepatic hemangioma. J Am Coll Surg. 2003; 197: 392-402. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12946794
- Erdogan GD, Busch OR, Van Delden OM, Bennink RJ, ten Kate FJ, et al. Management of liver hemangiomas according to size and symptoms. J Gastroenterol Hepatol. 2007; 22: 1953-1958. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17914976
- Hoekstra LT, Bieze M, Erdogan D, Roelofs JJ, Beuers UH, et al. Management of giant liver hemangiomas: An update. Expert Rev Gastroenterol Hepatol. 2013; 7: 263-268. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23445235
- Schnelldorfer T, Ware AL, Smoot R, Schleck CD, Harmsen WS, et al. Management of giant hemangioma of the liver: resection versus observation. J Am Coll Surg. 2010; 211: 724-730. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20980175
- Yedibela S, Alibek S, Muller V, Aydin U, Langheinrich M, et al. Management of Hemangioma of the Liver: Surgical Therapy or Observation? World J Surg. 2013; 37: 1303-1312. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23354918
- Herman P, Costa MLV, Machado MAC, Pugliese V, D'Albuquerque LAC, et al. Management of Hepatic Hemangiomas: A 14-Year Experience. J Gastrointest Surg. 2005; 9: 853-859. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15985244
- Marcello D, Gregor S, Angelo D, Karl O. The risk of spontaneous rupture of liver hemangiomas: A critical review of the literature. J Hepatobiliary Pancreat Sci. 2011; 18: 797-805. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/21796406
- Giuliante F, Ardito F, Vellone M, Giordano M, Ranucci G, et al. Reappraisal of surgical indications and approach for liver hemangioma: single-center experience on 74 patients. Am J Surg. 2011; 201: 741-748. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20937504
- Zhang W, Huang ZY, Ke CS, Wu C, Zhang ZW, et al. Surgical Treatment of Giant Liver Hemangioma Larger Than 10?cm: A Single Center's Experience with 86 Patients. Medicine (Baltimore). 2015; 94: e1420. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26313792
- Bajenaru N, Balaban V, Savulescu F, Campeanu I, Patrascu T. Hepatic hemangioma- review. J Med Life. 2015; 8: 4-11. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/26361504