More Information
Submitted: 28 August 2019 | Approved: 05 September 2019 | Published: 06 September 2019
How to cite this article: Islam SR, islam M, Sarkar SA, Paran S. Outcome of laparoscopic varicocelectomy with mass ligation technique for symptomatic varicocele. Arch Surg Clin Res. 2019; 3: 065-069.
DOI: 10.29328/journal.ascr.1001037
Copyright License: © 2019 Islam SR, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Varicocele; Laparoscopic varicocelectomy; Mass ligation; Recurrence
Outcome of laparoscopic varicocelectomy with mass ligation technique for symptomatic varicocele
Sardar Rezaul Islam1*, Majedul islam2, Shah Alam Sarkar3 and Shah Paran4
1Professor and Senior Consultant, Imperial Hospital, Chittagong, Bangladesh
2Assistant Professor, Department of Surgery, Jahurul Islam Medical College Hospitals, Bajitpur, Kishoreganj, Bangladesh
3Registrar, Imperial Hospital, Chittagong, Bangladesh
4Registrar, Jahurul Islam Medical College Hospital, Kishoreganj, Bajitpur, Bangladesh
*Address for Correspondence: Sardar Rezaul Islam, Professor and Senior Consultant, Imperial Hospital, Chittagong, Bangladesh, Tel: +8801746603305; Email: [email protected]
Background: Varicocele therapy is a controversial issue. No single approach is adopted as the best therapeutic option. Testes get blood supply from testicular artery, cremasteric artery and artery to the vas deference. So ligation of testicular artery in the abdomen do not cause ischemia to the testis. This was already demonstrated in many studies. Classical Palomo varicocelectomy also consists of open ligation of testicular vessels in the retroperitoneum. En mass ligation of testicular vein and artery is technically easy and fast in laparoscopic varicocelectomy (LV). Chance of missing some veins are also less. Henceforth recurrence is also less. Recurrence and post-operative complications are high when only testicular vein is ligated by laparoscopy in the retroperitoneum. We wanted to see the outcome of laparoscopic varicocelectomy by mass ligation technique.
Methods: 56 patients of symptomatic varicoceles were included in the study from the outpatient services. Symptomatic varicoceles of grade 2 to grade 3 were operated from January 2012 till January 2019 over a period of 7(seven) years in Jahurul Islam Medical college Hospital. The patients were selected for dull pain and ugly veins not for infertility. All were operated by laparoscopy with en-mass ligation of testicular vein and artery in the retroperitoneum. They were followed up for a period of six months after surgery. We collected all the data in a retrospective manner.
Results: The average operation time was 27±3 minutes. Average post-operative hospital stay was 32±7 hours. There were no technical failures requiring conversion to open varicocelectomy. There was no incidence of hydrocele formation nor testicular atrophy. One patient of bilateral varicocele had 50% reduction of his varicocele. We considered this a recurrence. All other patient had complete reduction of varicocele. One patient developed hemo-peritoneum due to dislodgement of hemo-clip, which required laparotomy. He did not require any further surgery for his varicocele.
Conclusion: Laparoscopic varicocelectomy with mass ligation technique is safe, effective, less time consuming and easy to perform. Recurrence and post-operative complications are minimum. Plastic hemo-lock should be used rather than titanium heom-clip for ligation of testicular vessels. There is no incidence of testicular atrophy or any adverse effect on testis.
Varicocele is an abnormal dilatation of the veins of the pampiniform plexus. It occurs in 6% of children at age of ten, 13% of adolescents and 15% of males in the general population. However, varicocele has been observed in 35% of men with primary infertility and up to 80% of men with secondary infertility [1]. The detrimental effect of varicocele on spermatogenesis in the sub-fertile male is manifested by low sperm count, decreased sperm motility and low percentage of normal sperm morphology together or in different combinations. Although many men with varicocele can father children varicocele causes a progressive time-dependent decline in semen quality. In general, varicoceles do not regress spontaneously. Varicocelectomy is the most common surgical procedure for infertility in males. These include incisional ligation of the veins through the retroperitoneal, inguinal or sub inguinal approaches. Other advanced procedure includes percutaneous embolization and laparoscopy. The goal of treatment of the varicocele is to obstruct the refluxing venous drainage to the testis. No accessory veins or vene commitments should not be missed during ligation. That is the reason why Palomo did ligation of both testicular veins and artery in the retroperitoneum by incisional method. The potential complications of varicocelectomy are recurrence, hydrocele formation, and testicular atrophy [2].
Patients selection: Between January 2012 and January 2019 over a period of 7 years, 56 patients underwent LV for left-sided, right sided and bilateral grade 2 and grade 3 varicocele. Age of the patients ranges between 15 to 54 years. Patients were selected with symptoms of pain in the testis and visible dilated ugly veins. None of them were selected for infertility. Ultrasonography of the scrotum were done for all patients to see dilated testicular veins and to confirm the diagnosis.
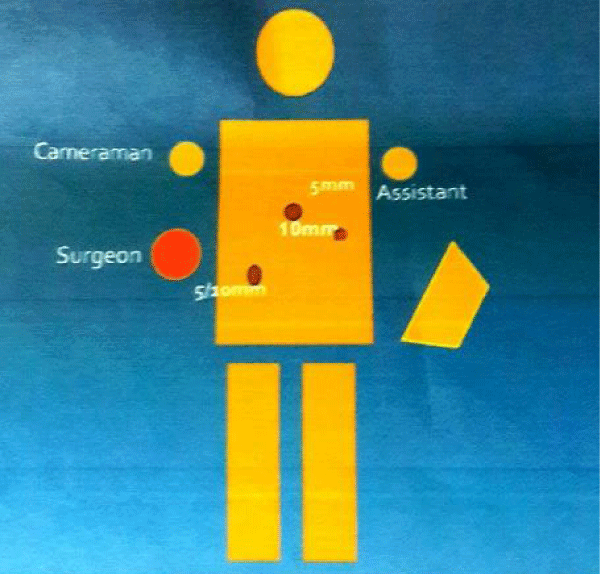
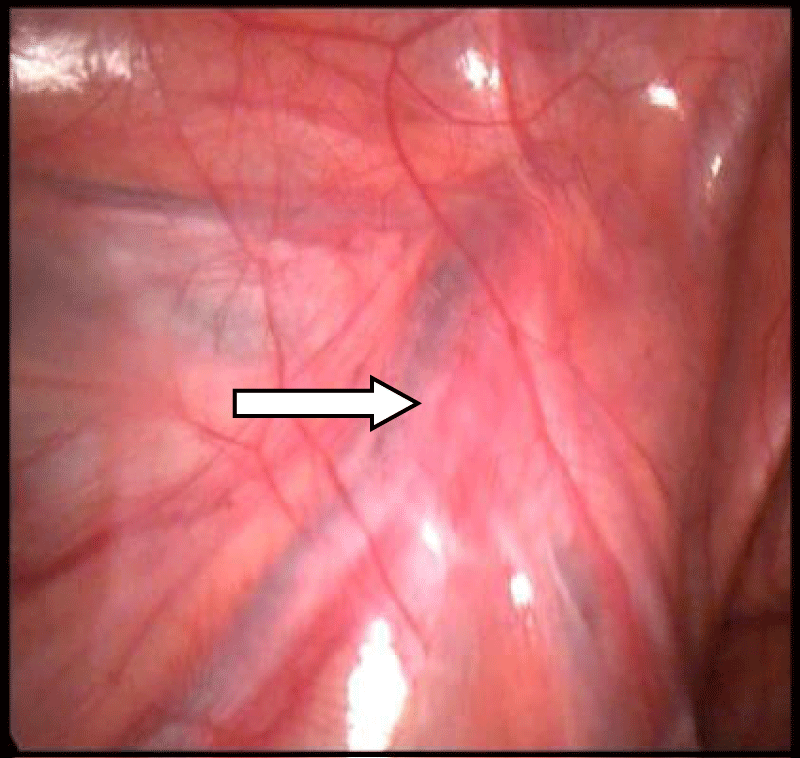
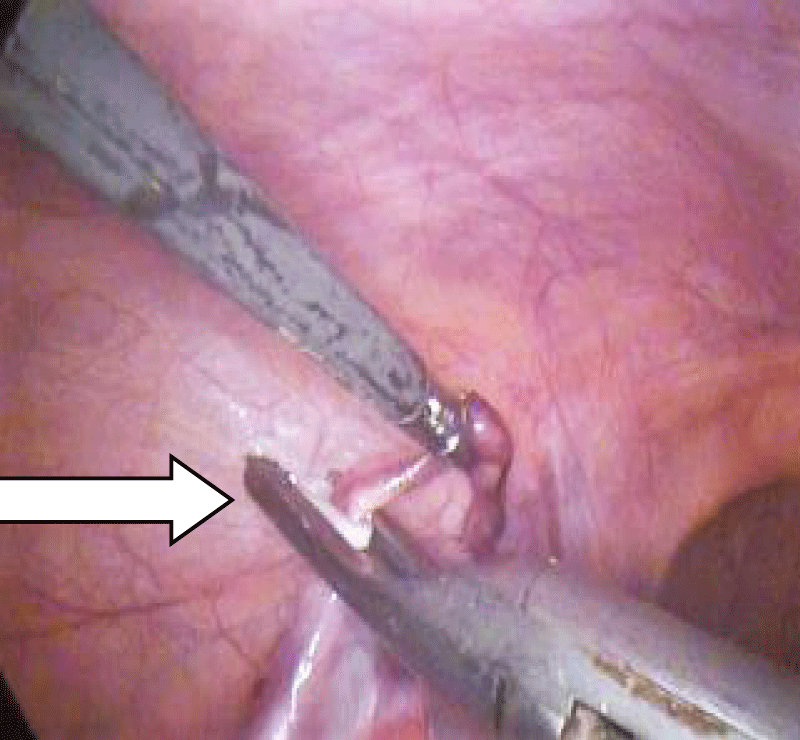
Operative technique-Patients were operated in supine position under general anesthesia. Three trocars were used for all cases. The first 10mm torcher was inserted just above the umbilicus. The second 10mm torcher was inserted on the upper right ileac fossa and the third 5mm trochar on the left midclavicular line slightly below the level of the umbilicus (Figure 1). 12 to 15mm pressure is used for maintenance of pneumo-peritoneum. The internal inguinal ring was identified by slight traction on the testis from outside. The traction on the testis causes visible traction of the peritoneum on the deep ring thus to help identify testicular vessels. Spermatic vessels and vas deferens become clearly visible from the deep ring (Figure 2). The retroperitoneum was incised with scissors along the internal spermatic vessels for approximately 1 to 2cm. After that the internal spermatic vessels were separated from the underlying psoas muscle with Maryland dissecting forceps. They were clamped with haemoclips. Usually four clips were applied on the vessels two centimeter apart. After an incidence of hemo-peritoneum two plastic hemo-lock were applied on either side of the excision ligation (Figure 3). The middle section of the spermatic vessel was excised and extracted via the right ileac fossa torcher. All the extracted specimens were sent for histopathology for confirmation (Figures 4,5).
The average operation time was 27±3 minutes. There was a single case of hemo-peritoneum which required laparotomy on 3rd post-operative day. There was no further complications afterwards. His varicocele was regressed as usual. There was no hydrocele formation nor recurrence in the post-operative follow-up period. The average hospital stay was 32±7 hours. Within one week of follow up all varicocele had marked reduction in size. At an average follow-up of 3 months, all patients remained asymptomatic. No recurrence seen during this 3 months follow up period. There were no testicular atrophy recorded during follow up period. Six patients developed testicular pain which were found to be due to concomitant epididimo-orchitis. They were all treated with proper antibiotic successfully. They did not have any residual pain after wards.
Figure 1: Ergonomics.
Figure 2: Laparoscopic view of testicular vessels.
Figure 3: Clipping of testicular vessel.
Figure 4: Left varicocele before surgery.
Figure 5: One week after mass ligation LV.
Traditional surgical correction of varicoceles has been done by ligation of the testicular veins via an inguinal (low/Ivanissevich) or retroperitoneal (high/Palomo) approach. However, these techniques in adolescents are associated with failure rates of approximately 3% to 37% [3]. Embolization of the testicular vein in experienced hands is reported to give better results, but recurrence still occurs in approximately 5% - 50% [4,5]. Also there is a 10 to 20% rate of unsuccessful intervention in the radiologic embolization approach. Venography has shown that the majority of missed vessels lie proximal to the site of vein ligation. In addition, the frequency of missed vessels is higher with a low approach. An approach that enables intraabdominal visualization of the testicular vessels might therefore be expected to reduce the rate of persistent or recurrent varicoceles. Limited data on laparoscopic management of varicoceles in adults give cure rates of 100%. These surprisingly good results may reflect the excellent visibility of the posterior abdominal wall achieved using the laparoscope, which allows a thorough search of sites known to be responsible for recurrent varicoceles, namely renal, vas associated, pelvic, and retro pubic cross-over veins. However, in patients who have recurrent varicoceles, the cause appears to be the presence of cremasteric or contralateral scrotal cross-over vessels, which conventional high and laparoscopic approaches may fail to control.
Hydrocele formation
Hydrocele formation is related to failure to preserve the lymphatic vessels associated with the spermatic cord. Franco suggests complication rates are relatively low for LVL except for the hydrocele rate, which has been similar to that encountered with the open Palomo approach in case of adolescent male [6]. Kandary, et al. [7], compared open Ingunal, laparoscopic and subinguinal microscopic (SMV) approach. They found that recurrence and hydrocele formation are least in the subinguinal microscopic approach. Recurrence rate of SMV, LV and Open technique are 5%, 13% and 18% respectively. Hydrocele formation of SMV, LV and open are 0%, 13% and 20% respectively. Again SMV needs expertise of microsurgical technique, which is not always available. Another study done by Mc Mnnus, et al. [8], which found that LV has less recurrence than SMV but higher rate of post-op hydrocele formation. Keys, et al. [9], had a hydrocele rate of 12.5%, Pini Prato, et al. [10], 12%, and Méndez-Gallart, et al. [11], 13.5% using laparoscopic mass ligation varicocelectomy.
Taneja et al. [12] has given and excellent comparison of recurrence and complication among all these four techniques in his book. He showed similar (6%) incidence of hydrocele formation in both mass ligation and artery preserving technique (Table 1). Astonishingly, we did not have any single incidence of hydrocele formation in our series.
| Table 1: Distribution of Varicoceles in our study | ||
| Left | Isolated Right | Bilateral |
| 47 | 1 | 8 |
Recurrence and testicular atrophy
Beck, et al. [13] suggested that unligated small internal spermatic veins may be a cause of varicocele recurrence. Rothman, et al. [14] also concluded that recurrences are due to either recollateralization or failure to ligate all branches of the venous plexus [14]. Keys, et al. [9] had a recurrence rate of 8.3% at their center doing laparoscopic mass ligation. Méndez-Gallart, et al. [11] showed that recurrence rates and complication rate of LV are similar to those reported with open surgery.
Testes get their blood supply from 3 sources. They are testicular artery from abdominal aorta, artery to the vas from internal spermatic artery and cremastereic artery from inferior epigastric aryery. So ligation of testicular artery should not cause testicular ischaemia as other two supply reamain present. Cimador, et al. [15] demonstrated that ligation of the artery does not impair testicular growth and thus it is more useful and safe to interrupt the artery to avoid recurrence due to periarterial venous network. Agnifilli, et al. [16] suggest that laparoscopic high mass ligation of both testicular artery and vein has very low recurrence rates and no incidence of testicular atrophy. Kattan, et al. [17] concluded that LVL with internal spermatic artery ligation has lower recurrence rate than without internal spermatic artery ligation with no increase in hydrocele or testicular atrophy rate. Our study also had no testicular atrophy and no hydrocele formation.
Polok, et al. [18] also concluded that varicocelectomy using clips gives much less complications than electrocoagulation and should be chosen first. We have also advocated the principle of applying clips throughout. We had one case of dislodgment of clip leading to hemo-peritoneum. Afterwards we used plastic hemo-lock onwards. Since then we did not have any bleeding complications. Tong, et al. [19] demonstated that lymphatic-sparing LV is a safe, effective and reliable treatment. Taneja, et al. [12] reorted about 2% recurrenece in Mass ligation and SMV technique but 11% in artery presrving and 6-11% in open inguinal technique. We had one case unsatisfactory reduction of varicocele in a bilateral varicocele. We considered this a recurrence (Table 2).
| Table 2: Comparison between LV(AP and ML), Open inguinal and SMV [12]. | |||
| Technique | Hydrocele % |
Atrophy % |
Recurrence % |
| LV-mass ligation | 6-7 | <1 | 2 |
| LV-Artery preserving | <6 | <1 | 11 |
| Open inguinal | 3-7 | <1 | 6-15 |
| SMV | <2 | <1 | <2 |
Improvement of semen quality and prengnancy rate
A major limitation of our study is we could not do semen analysis preoperatively and post-operatively to see the outcome of mass ligation laparoscopic varicocelectomy. Reason is these patients are mostly young, unmarried and did not present with infertility. They came for dragging testicular pain and ugly looking veins on the scrotum. So we did not go for semen analysis. But several literature analysis of outcome of both artery preserving and mass ligation varicocelectomy were found in literature.
Huk, et al. [20] and Parott, et al. [21] carried on comparative assessment of artery-ligating and artery-preserving varicocelectomy and found that ligation of vein and artery produced better improvement of semen characteristics and percentage of pregnancies in comparison with artery-sparing technique. Even Student, et al. [22] confirmed using colour Doppler sonography, that ligation of the testicular artery does not lead to major changes in testicular blood supply or sperm quality. Yamamoto, et al. [23] demonstrated the effect of varicocelectomy on post-operative spermatogenesis and showed that sperm density and motility improved significantly in the artery-ligated group. Yamamoto, et al. [23], Matsuda, et al. [24] and Fielder et al. [25] all of them concluded that in spite of the advocative advantage of artery preservation, there was no significant difference between artery-ligating and artery-preserving groups when improvements in semen quality and pregnancy rates were assessed. Ding, et al. [26] showed, in their randomized controlled trial with 1015 patient that LV is at intermediate position in improvement of spermatogenesis and rate of pregnancy. SMV was found to be most effective in improvement of semen quality and rate of pregnancy at one year. Open inguinal approach was found to be least effective. But SMV needs expertise in microvascular technique, which is not available in every center. On the otherhand LV is easy to perform, less time consuming and has short learning curve.
Laparoscopic varicocelectomy with mass ligation technique is safe, effective, less time consuming and easy to perform. Recurrence and post-operative complications are minimum. Plastic hemolock should be used rather than titanium heomclip for ligation of testicular vessels to avoid possible dislodgement of clip. There is no incidence of testicular atrophy nor any adverse effects on testis. LV should preferably be done with en-bloc mass ligation as it has least chance of recurrence.
- Oster J. Varicocele in children and adolescents: An investigation of the incidence among Danish school children. Scand J Urol Nephrol. 1971; 5: 27-32. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/5093090
- Kass EJ. Adolescent varicocele: Current concepts. Semin Urol. 1988; 6: 140-145. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5924953/
- Saypol DC. Varicocele. J Androl. 1981; 2: 61-71.
- Demas BE, Hricak H, McLure RD. Varicoceles: Radiologic diagnosis and treatment. Radiol Clin North Am. 1991; 29: 619-627. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/2024010
- Ayechu-Díaz A, Oscoz-Lizarbe M, Pérez-Martínez A, Pisón-Chacón J, Bento L. Treatment of adolescent varicocele: is percutaneous embolization better? Cir Pediatr. 2009; 22: 134-138. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19957860
- Franco I. Laparoscopic varicocelectomy in the adolescent male. Curr Urol Rep. 2004; 5: 132-136.
- Al Kandary AM, Shaban H, Ibrahim HM, Elshayebini YH, Shokeir AA. Comparison outcome of different varicocelectomy technique-open inguinal,laparoscopic and subinguinal microscopic varicocelectomy:a randomized clinical trial. Urology. 2007; 69: 417-420. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17382134
- Mc MnnusMC, Barqawi A, Meacham RB, Furness PD, Koyle MA. Laparoscopic varicocele ligation: are there advantages compared with the microscopic subinguinal approach? Urology. 2004; 64: 357-361. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15302494
- Keys C, Barbour L, O'Toole S, Sabharwal A. Laparoscopic surgery for varicoceles in children: an audit in a single centre. J Laparoendosc Adv Surg Tech A. 2009; 19: S107-109. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19371147
- Pini Prato A, MacKinlay GA. Is the laparoscopic Palomo procedure for pediatric varicocele safe and effective? Nine years of unicentric experience. Surg Endosc. 2006; 20: 660-664. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16432660
- Méndez-Gallart R, Bautista-Casasnovas A, Estevez-Martínez E, Varela-Cives R. Laparoscopic Palomo varicocele surgery: lessons learned after 10 years' follow up of 156 consecutive pediatric patients. J Pediatr Urol. 2009; 5: 126-131. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19083272
- Complications of Urology surgery, 4th Edition, S Taneja, Elsivier publication.
- Beck EM, Schlegel PN, Goldstein M. Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol. 1992; 148: 1190-1194. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1404635
- Rothman CM, Newmark H, Karson RA: The recurrent varicocele--a poorly recognized problem. Fertil Steril. 1981; 35: 552-556. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7227571
- Cimador M, Castagnetti M, Ajovalasit V, Libri M, Bertozzi M, et al. Sub-inguinal interruption of dilated veins in adolescent varicocele: should it be considered a gold standard technique? Minerva Pediatr. 2003; 55: 599-605. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/14676731
- Agnifili A, Schietroma M, Carlei F, De Berardis B, Pescosolido A, et al. Recurrences, testicular growth and semen parameters after laparoscopic Palomo varicocelectomy. Chir Ital. 2008; 60: 549-554. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18837256
- Kattan S. The impact of internal spermatic artery ligation during laparoscopic varicocelectomy on recurrence rate and short post-operative outcome. Scand J Urol Nephrol. 2001; 35: 218-221. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11487075
- Polok M, Patkowski D, Apoznański W, Dorobisz U, Laska E, et al. Electrocoagulation versus clips in laparoscopic varicocelectomy in boys. J Laparoendosc Adv Surg Tech A; 2009; 20: 277-280 PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19895211
- Tong Q, Zheng L, Tang S, Du Z, Wu Z, et al. Lymphatic sparing laparoscopic Palomo varicocelectomy for varicoceles in children: intermediate results. J Pediatr Surg. 2009; 44: 1509-1513. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/19635297
- Huk J, Fryczkowski M, Bihun M, Połać R. Laparoscopic varicocele ligation. The comparative assessment of artery-ligating and artery-preserving varicocelectomy. Wiad Lek. 2001; 54: 621-631. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11928549
- Parrott TS, Hewatt L. Ligation of the testicular artery and vein in adolescent varicocele. J Urol. 1994; 152: 791-793. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8022016
- Student V, Zátura F, Scheinar J, Vrtal R, Vrána J. Testicle hemodynamics in patients after laparoscopic varicocelectomy evaluated using color Doppler sonography. Eur Urol. 1998; 33: 91-93. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/9471047
- Yamamoto M, Tsuji Y, Ohmura M, Hibi H, Miyake K. Comparison of artery-ligating and artery-preserving varicocelectomy: effect on post-operative spermatogenesis. Andrologia. 1995; 27: 37-40. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7755188
- Matsuda T, Horii Y, Yoshida O. Should the testicular artery be preserved at varicocelectomy? J Urol. 1993; 149: 1357-1360. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8479036
- Fiedler U, Rost A. Studies on the reaction of the rabbit testis after ligation of the arteria and vena testicularis compared with ligation of the vein alone. Andrologia. 1976; 8: 351-354. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1008266
- Ding H, Tian J, Du W, Zhang L, Wang H, et al. Inguinal, laparoscopic or open microsurgical varicocelectomy for male infertility: a meta-analysis of randomized controlled trials. BJU Int. 2012; 110: 1536-1542.