More Information
Submitted: 07 April 2020 | Approved: 18 April 2020 | Published: 20 April 2020
How to cite this article: Karavdić K, Firdus A, Mešić A, Rahmanović S,Milardović R, et al. Laparoscopic-Assisted Transumbilical Extracorporeal Resection of Meckel’s Diverticulum in 10 years old boy with symptoms of gastrointestinal bleeding. Arch Surg Clin Res. 2020; 4: 006-010.
DOI: 10.29328/journal.ascr.1001044
ORCiD: orcid.org/0000-0002-7361-5212
Copyright License: © Karavdić K, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Diverticulum; Meckel; Laparascopic; Extracorporeal
Laparoscopic-Assisted Transumbilical Extracorporeal Resection of Meckel’s Diverticulum in 10 years old boy with symptoms of gastrointestinal bleeding
Karavdić K1*, Firdus A1, Mešić A2, Rahmanović S3, Milardović R4 and Đuran A5
1Clinic for Pediatric Surgery, Clinical Center of University Sarajevo, Bosnia and Herzegovina
2Clinic for Anesthesia and Reanimatology, Clinical Center of University Sarajevo, Bosnia and Herzegovina
3Gastroenterology Department, Pediatric Clinic, Clinical Center of University Sarajevo, Bosnia and Herzegovina
4Institute of Nuclear Medicine, Clinical Center of University Sarajevo, Bosnia and Herzegovina
5Clinic for Pathology, Clinical Center of University Sarajevo, Bosnia and Herzegovina
*Address for Correspondence: Kenan Karavdić, Clinic for Pediatric Surgery, Clinical Center of University Sarajevo, Sarajevo, Bosnia and Herzegovina, Tel: +38761202508; Email: [email protected]
The Meckel’s diverticulum (MD) is the most common anomaly of ductus omphaloentericus that surgeon encounters in clinical practice. The accurate incidence is unknown because most patients with the Meckel’s diverticulum are asymptomatic. Most studies report an incidence of about 2%. Approximately 4% of patients with the Meckel’s diverticulum become symptomatic.
A 10 years old boy, was sent from regional hospital. His symptoms started the day before he was hospitalized and represented as gastrointestinal bleeding, lower abdominal pain and four times vomiting, without fever. Ultrasound and X-ray of the abdomen were normal. Blood findings showed: RBC 3,19, hemoglobin 0,95, hematocrit 0,27. During a physical examination abdomen was palpatory soft, with no presence of the pain. Digital rectal examination showed blood. A scintigraphy pathologic scan showed a focal lesion of the right hemi abdomen consistent with the Meckel’s diverticulum.Patient was treated byLaparoscopic-Assisted Transumbilical Extracorporeal Resection of the Meckel’s Diverticulum.
The Meckel’s diverticulum is the most common anomaly of ductus omphaloentericus encountered in clinical practice. It is usually located on the antimesenteric border of the ileum within distance of 100 cm of the ileocecal valve [1]. The diverticulum has a blood supply from the vitellointestinal vessels located within the folds of the mesentery. Genuine diverticulum contains all three walls of the intestinal tract. The accurate incidence is unknown because the most of the patients who have Meckel’s diverticulum are asymptomatic. Most studies report an incidence of about 2% [2]. Approximately 4% of patients with Meckel’s diverticulum become symptomatic, meaning that 8 of them out of 10,000 will have complications [3]. The male-female complication ratio is about 3: 1,50% to 60% of all cases of symptomatic Meckel’s diverticulum that were detected within the first 2 years of life [4]. Symptomatic Meckel’s diverticulum ten times more often has heterotopic tissue (gastric, pancreatic and, less often, duodenal, colonial and biliary mucosa). 50% to 60% of the patients with ectopic tissue become symptomatic [5]. Complications aroused from Meckel’s diverticulum include gastrointestinal bleeding, intussusception, intestinal obstruction, abdominal pain and incarcerated hernia.
A 10 years old boy, was sent from regional hospital. Symptoms started the day before he was hospitalized and were presented as gastrointestinal bleeding, lower abdominal pain, four times vomiting, without fever. Ultrasound and X-ray of the abdomen were normal. Blood findings showed: RBC 3,19, hemoglobin 0,95, hematocrit 0,27. During a physical examination abdomen was palpatory soft, with no presence of the pain. Digital rectal examination showed blood (Figures 1,2).
Figure 1: Gastrointestinal bleeding and digital rectal examination.
Figure 2: Gastrointestinal bleeding and digital rectal examination.
Scintigraphy with radiopharmaceutical 20.6 mCi, Tc 99 pertechnetate with dynamic images of the abdominal and pelvic regions, taken for 60 minutes, and static imaging after 60 minutes, showed the focus of moderate accumulation in the right hemi abdomen, at the border of the upper and lower abdominal quadrants. The conclusion was that pathological scan shows a focal lesion of the right hemi abdomen consistent with the Meckel’s diverticulum (Figure 3). Pediatric gastroenterologist performed a distal rectoscopy 15 cm in length and has found only bloody content inside bowels without visible pathological changes (Figure 4).
Figure 3: Scintigraphy Tc 99 pertechnetate shows focal lesion of the right hemi abdomen consistent with the Meckel’s diverticulum.
Figure 4: Distal rectoscopy with bloody content in bowels.
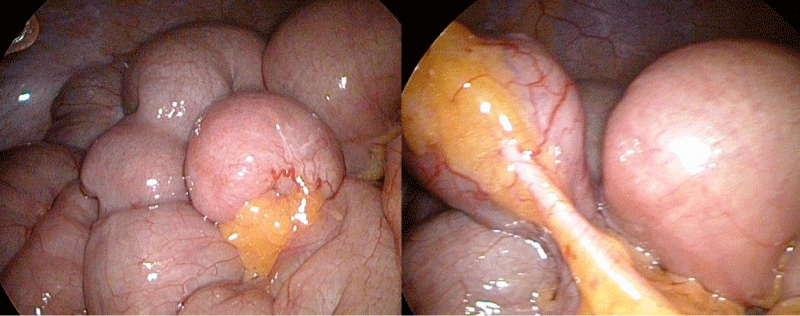
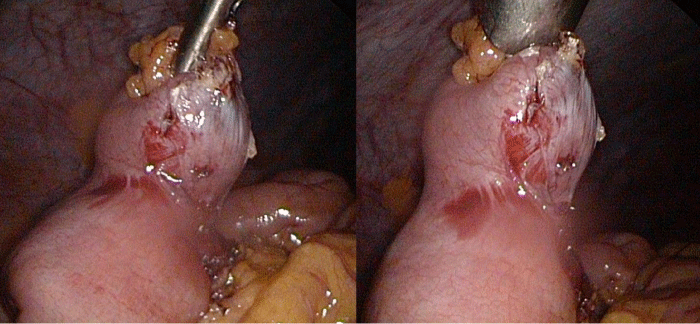
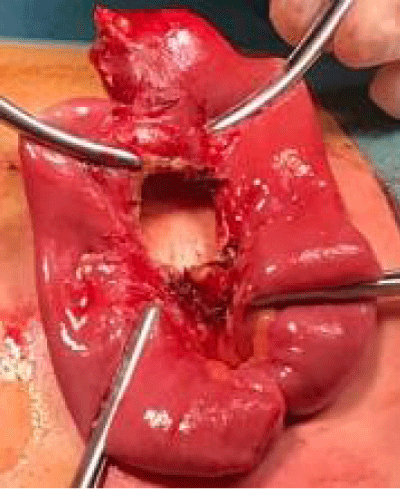
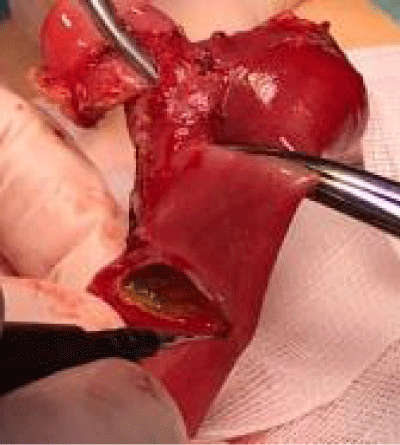
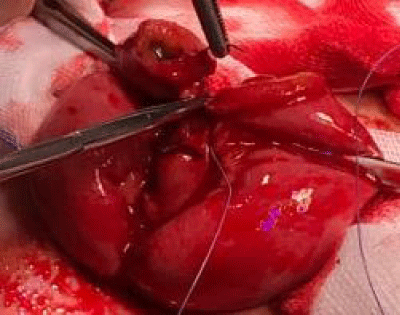
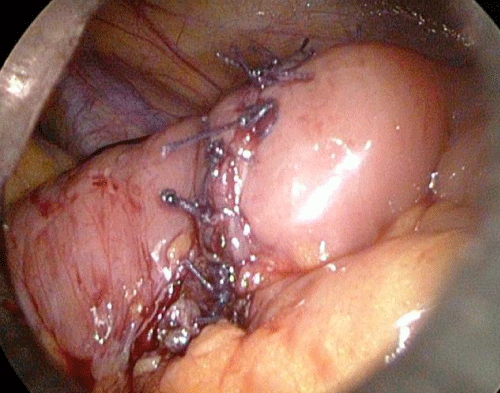
The procedure was performed under general anesthesia with an indwelling nasogastric tube and urinary catheter. After patient was put in convenient position and was prepared for procedure (surgical washing or operative field and surgical coverage) a 10 mm Hasson port was inserted using the open technique. Pneumoperitoneum was established based on the body weight, with an insufflation of 0.5/l/min to a maximum pressure of 12/mmHg. After systematic overview of the peritoneal cavity with a 10 mm operative telescope, two more 5-mm working ports were inserted. Systematic exploration of the small intestine was performed in a retrograde fashion from the caecum. The intestinal loops were thoroughly examined with an evaluation of the intestine on both sides of the mesentery. The Meckel’s diverticulum was directly identified, (Figures 5,6), grasped (Figure 7) and delivered through the umbilical port. The diverticulectomy was performed extra corporeally with intestinal resection/anastomosis, performed along with a sleeve of the adjacent ileum (Figures 7-11).
Figure 5: Laparoscopic view of Meckel’s diverticulum.
Figure 6: Meckel’s diverticulum grasped and delivered through umbilical port.
Figure 7: Exteriorization of the giant Meckel’s diverticulum through the umbilical port and extracorporeal resection.
Figure 8: Exteriorization of the giant Meckel’s diverticulum through the umbilical port and extracorporeal resection.
Figure 9: Resection and end to end anastomosis.
Figure 10: Resection and end to end anastomosis.
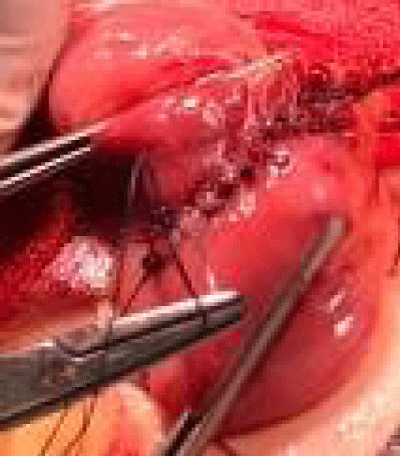
Figure 11: Completed hand-sewn end to end anastomosis after diverticulectomy. The intestine relocated in the abdominal cavity.
The intestine was then returned in the abdominal cavity, and the umbilical incision was closed with interrupted sutures, using 2-0 polyglactin to approximate the fascia.
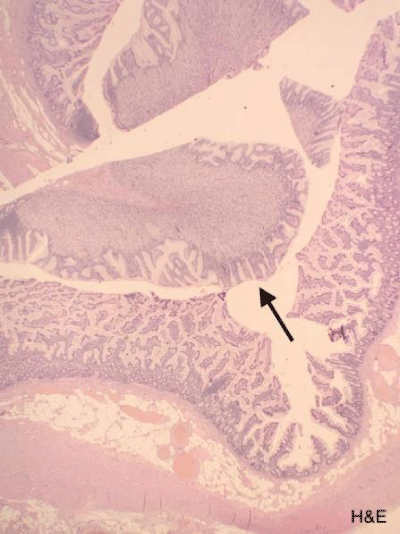
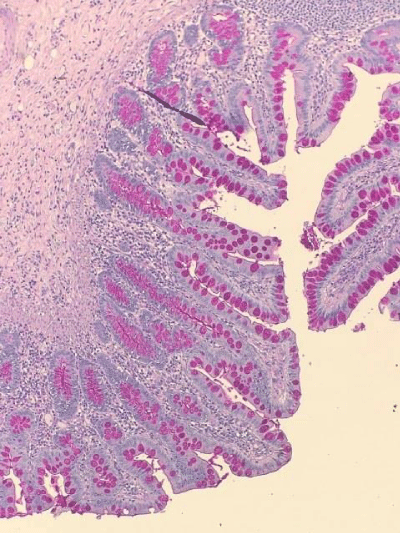
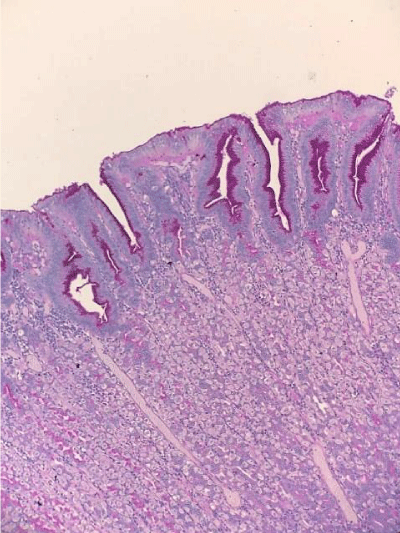
Histopathological findings
Diverticulum 27 mm long, 19 mm wide in diameter. In the diverticulum, the mucosa contains a vaguely restricted node, grayish in color, and measuring 16 x 15 x 12 mm. The mucous membrane of the stomach is permeated with a chronical inflammatory infiltrate of moderate intensity. Congested blood vessels are found in submucosal layer (Figures 12-16).
Figure 12: Completed hand-sewn end to end anastomosis after diverticulectomy. The intestine relocated in the abdominal cavity.
Figure 13: Histopathological findings: Meckel’s diverticulum specimen showing ectopic gastric mucosa of corporal type (black arrow).
Figure 14: Histopathological findings: Periodic acid–Schiff staining of small bowel mucosa.
Figure 15: Periodic acid–Schiff staining of gastric mucosa.
Figure 16: Abdominal wall and port entry points.
The postoperative course was uneventful. The patient had no fever, the peristalsis was established normally. The antibiotic Metronidasol was administered. On the 4th postoperative day, laboratory findings were analyzed and the patient was discharged from the hospital. The wound was normal and the patient’s sutures were removed on the 8th postoperative day.
Laparoscopy is first line procedure for diagnosing cases of complications due to MDs painless large intestinal bleeding. Tc99 scan has a reported sensitivity of 25% - 92% [6]. This diagnostic technique is the best non-invasive method for pre-operative diagnosis of MD. Menezes, et al. [7] conducted a retrospective review on the various presentations of symptomatic MD and assessed the sensitivity of the Meckel’s scan as a diagnostic tool in patients with gastrointestinal bleeding. They showed a sensitivity of 66.6% with a false negative rate of 33, 3%. In our case, scintigraphy showed accumulation of radiopharmaceuticals in the lower right abdomen, which confirmed a suspected Meckel’s diverticulum
Meckel’s diverticulectomy can be performed either intracorporeally or extra corporeally. Intracorporeal diverticulectomy can be performed totally laparoscopically without the need to enlarge the umbilical wound. The use of endoscopic staplers was the most frequent reported device used in diverticulectomy [10]. Schier, et al. [11] reported the use of endoloop and divided the diverticulum as in appendectomy. The early reports on laparoscopic assisted diverticulectomy favored the intracorporeal method. One of the concerns in total laparoscopic intracorporeally diverticulectomy was failure to perform segmental resection of Meckel’s diverticulum. Isolated diverticulectomy bears the risk of leaving ectopic gastric mucosa in the adjacent ileum.
In extracorporeal diverticulectomy, the Meckel’s diverticulum was delivered through an enlarged umbilical wound. Segmental resection of the Meckel’s diverticulum and the adjacent ileum were carried out. Hand-sewn small to small intestine anastomosis was performed [12]. The use of expensive laparoscopic staplers was avoided [13]. Ng, et al. [14] described the use of laparoscopic assisted extracorporeal Meckel’s diverticulectomy with endo GIA stapler and side-to-side ileal anastomosis. However, this method did not gain popularity.
Attwood, et al. [15], first described laparoscopic Meckel’s diverticulectomy by extracorporeal transumbilical resection with transverse application of the stapler at the diverticular neck. This procedure carries the risk of leaving heterotopic mucosal tissue, and the resection of the adjacent bowel is considered the treatment of choice today. In our case patient was treated by wedge or intestinal resection/anastomosis.
Altinli, et al. [16] reported extracorporeal transumbilical resection of the MD with hand-sewn anastomosis. This procedure has the benefits of palpation of the base of the MD for ectopic epithelium and also avoids the use of staplers, which are expensive and difficult to procure during an emergency. We applied the procedure recommended by Altinli, laparoscopically assisted extracorporeal resection, with end to end anastomosis done manually. We find the procedure easy to perform. The downside is the minimal increase in the umbilical aperture and the length of the procedure. The advantages of Atinli’s procedure over intracorporeal endoloop or stapler (EAG) and extracorporeal stapler resection are: the procedure is less expensive because it avoids the use of expensive staplers and the removal of ectopic mucosa, which may also occur at the resecting margins of the ileum.
The incidence of heterotopic mucosa in cases with MD varies between 15%-50% [9]. Shalaby, et al. [13] reported that the incidence of diverticular heterotopic gastric mucosa in symptomatic patients was 77, 8%. It is reported that heterotopic mucosa in symptomatic patients is much higher than in patients with asymptomatic MD. In the symptomatic patients, ectopic mucosa is present in 61% - 80% of cases and in only 13%-30% of incidental cases [9]. In our case, our patient was symptomatic, had gastrointestinal bleeding and ectopic gastric mucosa.
Park, et al. [17] reported the Mayo clinic experience with 1476 patients with Meckel’s diverticulum. The study included children and adult and did not specifically define the approach of operation. Post-operative complication in the most of 100 resected diverticulums were 13% in symptomatic group and 20% in asymptomatic group It is reported that the rate for postdiverticulectomy adhesive intestinal obstruction could be as high as 10% to 15% in children [18]. Intraoperative complication after laparoscopic assisted diverticulectomy was never reported in the literature. Sai Prasad, et al. [19] reported 8% of patients had intestinal obstruction after the operation. He suggested that the adhesion is secondary to ischemic bowel after release of the obstruction. Other studies did not show any intestinal obstruction post-operatively [20]. They all concluded laparoscopic assisted Meckel’s diverticulectomy was safe and feasible with good outcome. Our patient in the case report had excellent outcome and had no complications.
Laparoscopic-Assisted Transumbilical Extracorporeal Meckel’s Diverticulectomy performed without the use of expensive laparoscopic staplers is manually made anastomosis is a simple, safe, effective, and economic procedure which achieves a better cosmetic outcome.
Complete excision of the diverticulumand the adjacent intestine containing ectopicmucosa is essential to minimize the chance of recurrence.
- Chan KW, Lee KH, Wong HY, Tsui SY, Wong YS, et al. Laparoscopic excision of Meckel's diverticulum in children:What is the current evidence? World J Gastroenterol. 2014; 20: 15158-15162. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25386065
- Papparella A, Nino F, Noviello C, Marte A, Parmeggiani P, et al. Laparoscopic approach to Meckel's diverticulum. World J Gastroenterol. 2014; 20: 8173-8178. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25009390
- Prasad TR, Chui CH, Jacobsen AS. Laparoscopic-Assisted Resection of Meckel’s Diverticulum in Children. JSLS. 2006; 10: 310–316. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17212886
- Varcoe RL, Wong SW, Taylor CF, Newstead GL.Diverticulectomy is indequate treatment for short Meckel’s diverticulum with heterotopic mucosa. ANZ J Surg. 2004; 74: 869-872. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15456435
- Vane DW, West KW, Grosfeld JL. Vitelline duct anomalies. Experience with 217 childhood cases. Arch Surg. 1987; 122: 542-547. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/3495250
- Sai Prasad TR, Chui CH, Singaporewalla FR, Ong CP, Low Y, et al. Meckel’s diverticular complications in children: is laparoscopy the order of the day? Pediatr Surg Int. 2007; 23: 141-147. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17171378
- Menezes M, Tareen F, Saeed A, Khan N, Puri P. Symptomatic Meckel’s diverticulum in children: a 16-year review. Pediatr Surg Int. 2008; 24: 575-577. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18322689
- Rashid OM, Ku JK, Nagahashi M, Yamada A, Takabe K. Inverted Meckel’s diverticulum as a cause of occult lower gastrointestinal hemorrhage. World J Gastroenterol. 2012; 18: 6155-6159. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23155346
- Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV, Kavalakat AJ. Laparoscopic management of symptomatic Meckel’s diverticula: a simple tangential stapler excision. JSLS 2008; 12: 66-70. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18402742
- Teitelbaum DH, Polley TZ Jr, Obeid F. Laparoscopic diagnosis and excision of Meckel’s diverticulum. J Pediatr Surg. 1994; 29: 495-497. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8014801
- Schier F, Hoffmann K, Waldschmidt J. Laparoscopic removal of Meckel’s diverticula in children. Eur J Pediatr Surg. 1996; 6: 38-39. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8721178
- Chan KW, Lee KH, Mou JW, Cheung ST, Tam YH. Laparoscopic management of complicated Meckel’s diverticulum in children: a 10-year review. Surg Endosc. 2008; 22: 1509-1512. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18322735
- Shalaby RY, Soliman SM, Fawy M, Samaha A. Laparoscopic management of Meckel’s diverticulum in children. J Pediatr Surg. 2005; 40: 562-567. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15793736
- Ng WT, Wong MK, Kong CK, Chan YT. Laparoscopic approach to Meckel’s diverticulectomy. Br J Surg. 1992; 79: 973-974. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1422773
- Attwood SE, McGrath J, Hill AD, Stephens RB. Laparoscopic approach to Meckel’s diverticulectomy. Br J Surg. 1992; 79: 211. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/1532525
- Altinli E, Pekmezci S, Gorgun E, Sirin F. Laparoscopy-assisted resection of complicated Meckel’s diverticulum in adults. Surg Laparosc Endosc Percutan Tech. 2002; 12: 190-194. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/12080263
- Park JJ, Wolff BG, Tollefson MK, Walsh EE, Larson DR.. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950-2002). Ann Surg. 2005; 241: 529-533. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15729078
- Amoury R, Snyder C. Meckel’s diverticulum. Pediatric surgery. Louis: Mosby, St., 1988; 1173-1184.
- Sai Prasad TR, Chui CH, Singaporewalla FR, Ong CP, Low Y, et al. Meckel’s diverticular complications in children: is laparoscopy the order of the day? Pediatr Surg Int. 2007; 23: 141-147. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17171378
- Teitelbaum DH, Polley TZ Jr, Obeid F. Laparoscopic diagnosis and excision of Meckel’s diverticulum. J Pediatr Surg. 1994; 29: 495-497. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/8014801