More Information
Submitted: December 13, 2020 | Approved: December 30, 2020 | Published: December 31, 2020
How to cite this article: Onofrio L, Iarrobino G. Laparoscopic approach for acute right iliac fossa pathology: Our experience. Arch Surg Clin Res. 2020; 4: 054-058.
DOI: 10.29328/journal.ascr.1001055
ORCiD: orcid.org/0000-0001-6503-8796
Copyright License: © Onofrio L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Laparoscopic appendicectomy; Abdominal pain; Right iliac fossa; Complicated appendicectomy
Laparoscopic approach for acute right iliac fossa pathology: Our experience
Luciano Onofrio* and Gianfausto Iarrobino
Department of General, Oncological and Laparoscopic Surgery, Civil Hospital A.G.P., Italy
*Address for Correspondence: Luciano Onofrio, Department of General, Oncological and Laparoscopic Surgery, Civil Hospital A.G.P. Piedimonte Matese, Via Matese 1– 81016, Italy, Email: [email protected]
Laparoscopic approach in emergency theatre is an irreplaceable tool to manage patients with acute surgical pathology. We retrospectively reviewed surgical access records from the Emergency Department for acute right iliac fossa pathology. We considered 51 patients (16 male, 35 female, mean age 23.8 years) access for acute right iliac fossa pathology over the last year. 44 patients underwent laparoscopic approach (86%); 8 patients were treated with an open approach. Outcomes evaluation was based on data comparison from open appendicectomy over 4 year time period.
Variables considered for data analyses were: role of laparoscopic surgery for gangrenous/perforated appendicitis, Conversion rate, Laparoscopy appendicectomy for elderly patients.
Our study demonstrated that a laparoscopic approach at acute right iliac fossa pathology is feasible, safe and can offer a low incidence of infectious complications, less post-operative pain, rapid recovery, and represent a valid diagnostic tool in doubtful cases, at the expense of longer operating time than OA. We suggest that LA should be the initial choice for all patients with acute right iliac fossa pathology.
Laparoscopic approach (LA) in emergency theatre is an irreplaceable tool to manage patients with acute surgical pathology. This approach can be, in doubtful cases, the last diagnostic act and the first therapeutic one. Women affected by pelvic pain of unclear origin constitute a paradigmatic example: laparoscopy can point out diagnosis and, if necessary, treat it with minimal trauma, low invasiveness and small surgical wounds.
Nowadays, LA maintains all the advantages of elective laparoscopic surgery (low invasiveness, better postoperative course, better cosmetic results with a rapid return to activity), combined with most of therapeutic options of an Open Approach (OA).
The appendix represents, unquestionably, the main component in pathologies of the right iliac fossa. Among surgical pathologies, the appendix represents the first cause of acute abdomen and appendectomy is the most frequent surgical procedure practiced in Emergency departments. Moreover, its presentation is often very variable, such as the site of pain, the bimodal incidence curve, atypical signs and symptoms, which can complicate the correct management of this pathology [1]. Concerning anatomic peculiarities of right iliac fossa, laparoscopy allows complete exploration of the peritoneal cavity; treatment of surgical such as gynecological pathologies, correct focalization of mismatched or rare causes of abdominal pain [2].
Knowledge of the main pathways of acute abdominal pain is an essential tool for a correct interpretation of symptoms and physiopathology, which in turn are essential aspects for a rapid and correct treatment.
We retrospectively reviewed surgical access records from the Emergency Department for acute right iliac fossa pathology. Access records from 1of January to 31 December 2019 were consulted. We considered 51 patients (16 male, 35 female, average age 23.8 years). 44 patients underwent laparoscopic approach (86%); 8 patients were treated by open approach (included 2 patients converted to open surgery – 4,5%). Operative time range was 28 – 96 min (median 62 min). All patients underwent blood examinations, abdomino-pelvic US; TC scan was perform in 25 pz (49%); gynecological evaluation was performed in all women; Endovaginal ultrasound examination was performed in 26/35 patients (74%).
Histological examination documented: 36 acute appedicitis (20 acute catharralis, 12 acute suppurative, 4 gangreous/perforated appendicitis); 3 gynecological pathology, 3 nopathological appendix.
Concerning patients converted to open appendectomy (2 patients – 4.5%), in both cases perforated appendicitis with abscess and severe acute inflammatory process were observed; the lack of clear anatomical landmarks and substantial progress in surgery after 30 mins. were judged valid criteria for conversion.
In three cases, gynecological alteration were the result of laparoscopic exploration. In two cases with ovarian hemorrhagic cyst, with peritonitis in one case, were managed with marsupialization technique. The third case consisted in acute appendix with severe flogistic reaction that involved omentum causing an ovarian torsion by inflammatory attraction. Laparoscopic Adhesiolysis and appendicectomy were performed. Surprisingly one case of hemorrhagic cyst and the one concerning ovarian torsion were diagnosed with “no pathological alterations at gynecological tract” at gynecological evaluation.
Concerning “white appendix” (3 pz – 5.7%): two patients showed no pathological alterations except adhesions in right iliac fossa between organs (colon, appendix and abdominal wall); they never underwent surgical procedure and had a reported clinical history of recurrent abdominal pain of more than 6 months. One case presented a relevant citrine peritoneal effusion without other finding.
All these patients were approached with appendicectomy, added with adhesiolysis in the first two cases. Histological examination documented mucosal inflammation (2 pz) and a stool appendix obstruction (1 pz).
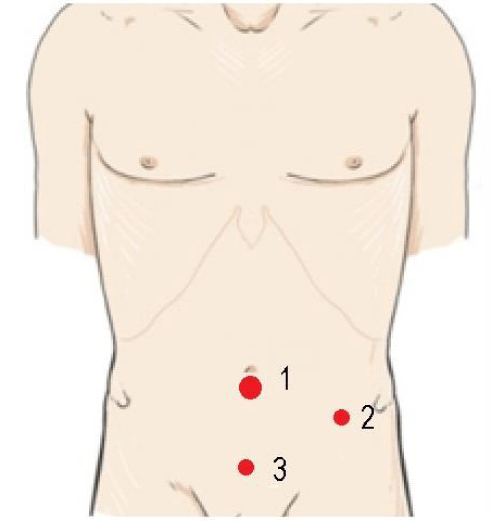
LA is based on a 3 trocars approach: one umbilical (10 mm), one suprapubic (5 mm), one (optic) at left iliac fossa (5 mm) as shown in figure 1. Reusable material used includes: grasping forceps, bipolar forceps, scissors, needle holders. Operative extractor bags, clips, staples or harmonic energy instruments are unnecessary. The surgeon is on the left side of the patient, with the first assistant on his right and instrumentation table on the left. The monitor is on the right side of the patient.
Figure 1: Trocar size and disposition: 1 umbilical 10 mm, 2 optic 5 mm, 3 operative 5 mm.
The surgical technique consists of the following steps:
1) To hold the ileocecal appendix with grasping forceps introduced through suprapubic trocar;
2) Use of bipolar forceps to isolate the appendix from its meso, coagulate the appendiceal mesentery and skeletonize the appendix;
3) Use of needle holders to “close” the base of the appendix with 2 pre-formed loops of absorbable threads.
4) To “seal’’ the distal part of the sutured appendix with bipolar forceps to avoid leakage of the contents of the appendix
5) To cut the suture thread at the appendix base.
6) Removal of the appendix by, pulling the grasping forceps, after section, into the umbilical 10mm trocar. It’s withdrawn from the abdominal wall (with the appendix inside) to avoid the risk of contamination of the abdominal cavity and wall.
7) To “coagulate” mucosa of appendiceal stump (with bipolar forceps) to avoid mucosa resection side being exposed in the intraabdominal cavity, causing leakage of infected substances and increasing intra-abdominal abscess.
8) To wash the abdominal cavity and the application of abdominal drainage (18 f) in cases of complicated appendicitis (17/44 pz), going out through suprapubic trocar incision, generally removed in the first 24 hours.
The surgical technique in laparotomic approach (OA) is mostly represented by a Stropeni way of access (cutaneous Mac Burney and right para-rectal incision of the muscles), after gaining the abdominal cavity and identified appendix: isolate it from its meso; double ligation by absorbable threads, of meso and appendix, section between the threads of both structures, make an oversuture on the cecum around the appendiceal stump doing its invagination [3].
Outcomes evaluation has compared data from open Appendicectomy over the last 4 years (2016-2019: 113 cases) to Laparoscopic appendicectomy during the last year (2019).
There were statistically significant differences in operative time between the LA and OA group: 62 vs. 45 minutes | p < 0.05.
Pain after LA on the first postoperative day was significantly less (we considered analgesic number of request/24 h LA = 0.4| OA = 0.8) except in the early Post-Operative time (6 h) where no differences were higtlighted. No relevant differences were present in patients affected by gangrenous/perforated appendicitis in both groups.
Concerning the rate of complications, wound infection after LA was undeniably reduced (LA: 5.0% | OA: 9.0%) such as postoperative ileus; in addition an earlier resumption of normal diet, a shorter hospitalization (LA: 2.9 days | OA: 4.1 days), a more rapid recovery to resume normal activities emerged for LA as compared to OA.
Analysis of the incidence of intra-abdominal abscess (LA = 4.54% | OA = 8.84%) did not show any significant differences. Treatment was conservative in all cases in LA Group; there were 2 cases managed by surgical treatment in OA.
In the context of the “acute abdomen” we have to consider a large and heterogeneous group of different pathologies that can schematically be classified in:
1. T.A.S.( take advantage of surgery).
2. T.A.D. (take advantage of drugs).
The first group includes all cases requiring a surgical treatment to be solved; without considering traumatic and iatrogenic causes, our specific group (acute right iliac fossa pathology) included: acute appendicitis, acute diverticulitis, ectopic pregnancy, follicular cyst, endometriosis, Pelvic Inflammatory Disease, intestinal occlusion, Merkel diverticulum, etc.
The TAD’s Group comprises:
N.S.A.P. (nonspecific abdominal pain): defined as a pain going on for 7 days or less with uncertain diagnosis after diagnostic based tests. Despite numerous attempts to develop shared diagnostic algorithms, evidence-based clinical guidelines for the management of this nosological entity are currently not available [4-6].
F.A.D. (false acute abdominal): a group of pathologies, of internistic interest, which simulate a clinical context of an acute abdomen, such as:
Nervous system diseases (herpes zoster, syphilis, slipped disc, etc...).
Metabolic diseases (diabetes, Addisonian crisis, hyperthyroidism, etc...).
Hemopathies (drepanocytic anemia, paroxysitic nocturnal hemoglobinuria, coagulopathies, etc...).
Collagenopathies (R.F. Les, Schoenlein-Henoch purpura, etc...).
Toxic diseases (heavy metals intoxication, botulism, Mushroom poisoning,narcotic suspension).
Hereditary diseases (acute intermittent porphyria, familial type I hyper-lipo-proteinemia, hereditary angioedema, etc...) [7,8].
We have to consider that non-surgical causes of acute abdominal pain simulating an acute abdomen account for up to 30% of patients requiring hospital admission, therefore it is relevant for the treatment of acute surgical pathologies [21,22].
This complex situation makes the need for a useful approach to define the diagnosis and subsequent treatment. This approach can surely be laparoscopy given that L.A. can be considered the first choice in suspected appendicitis, especially in women. In such patients, in presence of acute right iliac fossa pain, differential diagnosis between acute appendicitis, ectopic pregnancy and pelvic inflammatory disease (PID), is necessary. A laparoscopic exploration of the abdominal cavity allows a rapid and safe diagnosis, it can represent a therapeutic option and can improve patient managing in certain cases (id P.I.D. cases) [10].
Some issues are still debated, and will be briefly examined here:
- The role of laparoscopic surgery for gangrenous and/or perforated appendicitis remains controversial due to concerns of an increased incidence of post-operative intra-abdominal abscesses (IAA). Our analysis showed that IAA, in complicated appendicitis, seems to be significantly reduced, even though statistical evidence needs to be confirmed given our numbers (LA: 4.54% | OA: 8.84%). However our findings are also corroborated by recent metanalysis [10-12,17].
We believe that, the procedure in complicated appendicitis contemplating: debridement, irrigation and lavage under direct visualization of the entire peritoneal cavity with (not less than) 6 liters of warm saline solution, greatly reduces the microbial load and concentration, resulting in a smaller percentage of IAA. However, pus collection in right paracolic gutter, pelvis or both, was found to be predictive for IAA [13].
Moreover, clinical presentation of abdominal abscesses is varius and complex as the nature of abscesses. The range is vast: from a frank septic shock to nothing at all; potentially involving also immunoparesis, antibiotics, “partially treated” or “masked” situations. The same occurs for time of presentation, occasionally distant (weeks) from surgery.
Wound infection after LA was undeniably reduced (LA: 5.0 | OA: 9.0). The extraction of appendix through the trocar or inside a disposable bag (avoiding direct contact with wounds/skin) can account for this result [10].
- Conversion rate: According to literature, [11,15] conversion rate to open access was about 8%, given that the first cause of conversion is the presence of a severe inflammatory process, adhesions represent the second conversion cause [23]. These data are consistent with the conversion rate observed in our study (4.35%). However, other factors should be considered which my determine conversion, such as surgeon’s laparoscopic’s skills and his expertise with the laparoscopic approach, patient conditions in terms of comorbidity and the stability of vital signs during the procedure [10,18].
In our study, the old surgical aphorism “conversion = complication” turned out to be correct: the 2 patients converted to open access showed delayed canalization and IAA treated conservatively.
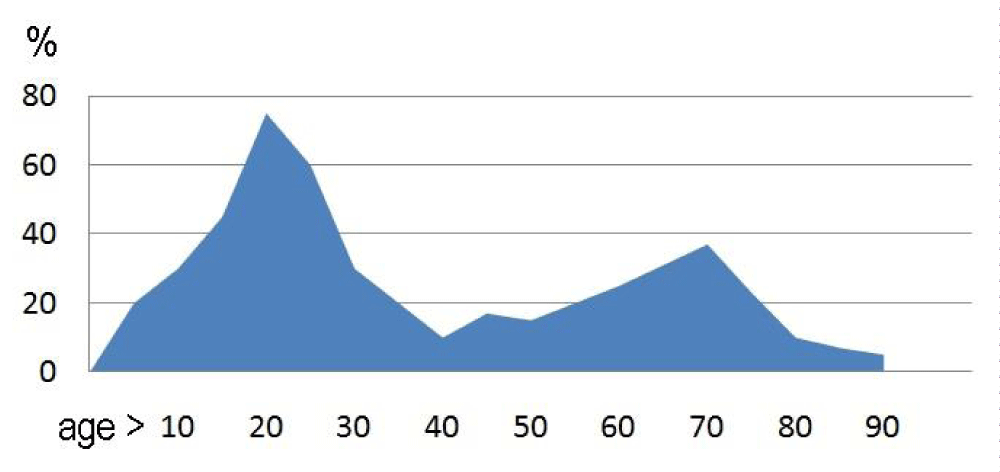
-Laparoscopy appendectomy for elderly patients: An acute appendicitis does not totally represent a disease in young people; however it is the second most common acute abdomen in patients ≥ 50 years of age, giving a typical bimodal incidence distribution for the disease (Figure 2) with a maximum peak in adolescence and a second, smaller peak in the elderly [7].
Figure 2: Bimodal age distribution of acute appendicitis incidence rates [24].
In the elderly, delayed treatments are the primary aggravating factor that impacts treatment outcome. Delayed diagnosis is caused by delayed patient admittance to the Emergency Department and stems from variable perceptions of pain in the elderly, difficulties in obtaining a complete patient history, or atypical symptoms [24].
Laparoscopy according to our data, seems to be a safe and feasible option and it is associated with decreased rates of post-operative morbidity and shorter hospitalization. However the limited consistency of this group of patients does not allow statistical evaluations in our study, but it is a trend consistent with evidence in literature [15,18,19].
-The operating time in our study was longer in LA than in OA (62 vs. 45 minutes | p < 0.05); which may be due to learning curve, time used for peritoneal lavage, associated procedures. Longer operating time of LA when compared with OA was also reported in many studies [15]. We do not consider this to a relevant factor in absolute terms, if compared with the undoubted advantages of the laparoscopic approach so far exposed.
-N.S.A.P.: nonspecific abdominal pain is not considered for a surgical approach. However we have treated 3 patients with acute abdominal pain at iliac right fossa (2 women aged 17 and 34 years, 1 man aged 15 years.) with a long history (> 1 year) of a specific generic abdominal pain (2 or more episodes/month) with episodic acute intensive pain. All of them underwent multiple and repeated diagnostic procedures, emergency room access and specialist visits, without reaching an effective diagnostic and therapeutic conclusion. Surgical findings result in adhesions in right iliac fossa (2 patients); they never underwent surgical procedure before. The last case presented a relevant citrine peritoneal effusion and no other finding. Histological examination documented mucosal inflammation (2 patients) and a stool appendix obstruction (1 patient). The most significant fact is represented by the complete resolution of their chronic symptoms at the 6-month follow-up in all cases. We believe that laparoscopic exportation of the abdomen could be considered as a valid tool in diagnostic and therapeutic protocol in selected cases of N.S.A.P. [20].
Chronic appendicitis (CA) the existence of chronic appendicitis appears to be controversial and divisive among many physicians. Recurrent appendicitis is defined as one or more episodes of acute appendicitis, usually, lasting 24–48 hrs, and it subsides on its own, whereas CA mainly presents as a less severe, nearly continuous abdominal pain lasting longer than the typical 1–2-day period, and often extending to weeks, months, or even years [25,26]. Conservative treatment of acute appendicitis, as a viable approach to apply to the non-operative management in a cohort of selected patients could lead to an increased number of these specific situations. Far from wanting to set a final claim on the existence of sub-acute or chronic appendicitis, laparoscopy could be considered as a diagnostic and therapeutic tool, aimed at solving chronic symptoms (often impacting on the quality of life of the affected people), also leading to a general cost reduction, such as those related to recurrent first aid access, diagnostics procedures and specialist visits.
In conclusion, our study demonstrates that laparoscopic approach at acute right iliac fossa pathology is feasible, safe and can offer a low incidence of infectious complications, less post-operative pain, rapid recovery, and may represent a valid diagnostic tool in doubtful cases, on the expense of longer operating time than OA. We suggest that LA should be the initial choice for all patients with acute right iliac fossa pathology.
Seneca said: “We have before us the sins of other men, but we carry ours on the back.’’ That we can, in surgery as in life, put our sins before those of others, so that others do not have to commit equal.
Declarations
- The authors have no relevant financial or non-financial interests to disclose
- The authors have no conflicts of interest to declare that are relevant to the content of this article
- All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript
- The authors have no financial or proprietary interests in any material discussed in this article
- Adiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. 1990; 132: 910-925. PubMed: https://pubmed.ncbi.nlm.nih.gov/2239906/
- Gans SL, Pols MA, Stoker J, Boermeester MA. Expert steering group. Guideline for the Diagnostic Pathway in Patients with Acute Abdominal Pain. Digest Surg. 2015; 32: 23-31. PubMed: https://pubmed.ncbi.nlm.nih.gov/25659265/
- Cariati A, Brignole E, Tonelli E, Filippi M, Guasone F, et al. Laparoscopic or open appendectomy. Critical review of the literature and personal experience. G Chir. 2001; 22: 353-357. PubMed: https://pubmed.ncbi.nlm.nih.gov/11816948/
- Arias MP, Barreira AS, Sánchez MM, Eire PF, Saavedra SG, et al. Appendicitis versus non-specific acute abdominal pain: Paediatric Appendicitis Score evaluation. An Pediatr. 2018; 88: 32-38. PubMed: https://pubmed.ncbi.nlm.nih.gov/28254168/
- Gans SL, Pols MA, Stoker J, Boermeester MA. Expert steering group. Guideline for the diagnostic pathway in patients with acute abdominal pain. Dig Surg. 2015; 32: 23-31. PubMed: https://pubmed.ncbi.nlm.nih.gov/25659265/
- Onur OE., et al. Follow-up ambulatoriale o “osservazione clinica attiva” in pazienti con dolore addominale aspecifico in pronto soccorso. Uno studio clinico randomizzato. Minerva Chirurgica. 2008; 63: 9-15.
- Royds Jones HM. The False "Acute Abdomen". 1951.
- Rathish D, Karalliyadda S. Concurrent presentation of thyroid storm and diabetic ketoacidosis: a systematic review of previously reported cases. BMC Endocr Disord. 2019; 19: 49. PubMed: https://pubmed.ncbi.nlm.nih.gov/31101104/
- Vetshev PS, Ippolitov LI, KOvalenko EI. False acute abdomen in clinical practice. Klin Med (Mosk). 2003; 81: 20-27.
- Ruffolo C, Fiorot A, Pagura G, Antoniutti M, Massani M, et al. Acute appendicitis: What is the gold standard of treatment? World J Gastroenterol. 2013; 19: 8799–8807. PubMed: https://pubmed.ncbi.nlm.nih.gov/24379603/
- Lin HF, Lai HS, Lai IR. Laparoscopic treatment of perforated appendicitis. World J Gastroenterol. 2014; 20: 14338–14347. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202363/
- Jaschinski T, Mosch CG, Eikermann M, Neugebauer EAM, Sauerland S Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018; 11: CD001546. PubMed: https://pubmed.ncbi.nlm.nih.gov/30484855/
- Melanie B, Saltzman DA, Rosen JI, Acton RD, Segura BJ, et al. Standardized irrigation technique reduces intraabdominal abscess after appendectomy. J Pediat Surg. 2019; 54: 728-732. PubMed: https://pubmed.ncbi.nlm.nih.gov/30025605/
- Domene CE, Volpe P, Heitor FA. Three port laparoscopic appendectomy technique with low cost and aesthetic advantage. Arq Bras Cir Dig. 2014; 27(Suppl 1): 73–76. PubMed: https://pubmed.ncbi.nlm.nih.gov/25409972/
- Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, et al. Laparoscopic Versus Open Appendectomy: Outcomes Comparison Based on a Large Administrative Database. Ann Surg. 2004; 239: 43-52. PubMed: https://pubmed.ncbi.nlm.nih.gov/14685099/
- Lim SG, Ahn EJ, Kim SY, Chung Y ll, Park JM, et al. A Clinical Comparison of Laparoscopic versus Open Appendectomy for Complicated Appendicitis. J Korean Soc Coloproctol. 2011; 27: 293-297. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3259425/
- Sakpal SV, Bindra SS, Chamberlain RS. Laparoscopic appendectomy conversion rates two decades later: an analysis of surgeon and patient-specific factors resulting in open conversion. J Surg Res. 2012; 176: 42-49. PubMed: https://pubmed.ncbi.nlm.nih.gov/21962732/
- Wang D, Dong T, Shao Y, Gu T, Xu Y, et al. Laparoscopy versus open appendectomy for elderly patients, a meta-analysis and systematic review. BMC Surgy. 2019; 19: 54.
- Kirshtein B, Perry ZH, Mizrahi S, Lantsberg L. Value of laparoscopic appendectomy in the elderly patient. World J Surg. 2009; 33: 918-922. PubMed: https://pubmed.ncbi.nlm.nih.gov/19172345/
- Decadt B, Sussman L, Lewis MP, Secker A, Cohen L, et al. Randomized clinical trial of early laparoscopy in the management of acute non-specific abdominal pain. Br J Surg. 1999; 86: 1383-1386. PubMed: https://pubmed.ncbi.nlm.nih.gov/10583282/
- Viniol A, Keunecke C, Biroga T, Stadje R, Dornieden K, et al. Studies of the symptom abdominal pain--a systematic review and meta-analysis. Fam Pract. 2014; 31: 517–529. PubMed: https://pubmed.ncbi.nlm.nih.gov/24987023/
- Sapmaz F, Başyiğit S, Başaran M, Demirci S. Non-Surgical Causes of Acute Abdominal Pain - Actual Problems of Emergency Abdominal Surgery. 2016.
- Peedikathara LM, Mandumpala JM, Vallon SM, Kavalakat AJ. Predictors for conversion to open appendicectomy in patients undergoing laparoscopic appendicectomy: a prospective study. Int Surg J. 2018; 5: 2588-2594.
- Malý O, Páral J. Appendicitis as a rare cause of mechanical small-bowel obstruction: A literature review of case reports. Int J Surg Case Rep. 2016; 29: 180-184. PubMed: https://pubmed.ncbi.nlm.nih.gov/27865147/
- Kothadia JP, Katz S, Ginzburg L. Chronic appendicitis: uncommon cause of chronic abdominal pain. Therap Adv Gastroenterol. 2015; 8: 160–162. PubMed: https://pubmed.ncbi.nlm.nih.gov/25949528/
- See TC, Watson CJE, Arends MJ, Ng CS. Atypical appendicitis: the impact of CT and its management. J Med Imaging Radiat Oncol. 2008; 52: 140-147. PubMed: https://pubmed.ncbi.nlm.nih.gov/18373805/