More Information
Submitted: December 24, 2020 | Approved: January 12, 2021 | Published: January 13, 2021
How to cite this article: Arabaci B, Ceylan KC, Ermete S, Kilic K, Kaya SO. Soliter fibrous tumor of diaphragm in a patient with larynx cancer: Case report. Arch Surg Clin Res. 2021; 5: 001-003.
DOI: 10.29328/journal.ascr.1001056
ORCiD: orcid.org/0000-0002-6609-2839
Copyright License: © Arabaci B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Soliter fibrous tumor of diaphragm in a patient with larynx cancer: Case report
Bengisu Arabaci*, Kenan Can Ceylan, Sulun Ermete, Devrim Kilic and Seyda Ors Kaya
University of Health Sciences, Department of Thoracic Surgery, Dr. Suat Seren Chest Diseases and Thoracic Surgery Training and Research Hospital, Turkey
*Address for Correspondence: Bengisu Arabaci, University of Health Sciences, Department of Thoracic Surgery, Dr. Suat Seren Chest Diseases and Thoracic Surgery Training and Research Hospital, Turkey, Tel: +905426042807; Email: [email protected]
Introduction: Solitary fibrous tumor is a neoplasm of mesenchymal origin with benign and malignant forms. We aimed to present a case of solitary fibrous tumor which developed in a patient operated for laryngeal cancer and originated from diaphragm in the light of the literature.
Case report: A 61-year-old male patient with tracheostomy with an undiagnosed lesion that appears to be almost 10 cm was referred to our clinic. Since it was a large volume mass, we chose to perform a thoracotomy over thorachoscopic approach.
Discussion: Although solitary fibrous tumors most commonly occur in the pleura but may also originated from diaphragm, and our case is valuable that originates from diaphragmatic since there are less than 5 reported cases in literature for past two decades.
Conclusion: Even in the case of recurrence, the main treatment remains as total surgical excision. Solitary fibrous tumors are usually detected because of compression symptoms. That is the main reason why we chose thoracotomy.
Solitary fibrous tumor (SFT) is a neoplasm of mesenchymal origin with benign and malignant forms [1]. It may be originated from the visceral pleura in the thoracic region, and as well as from the diaphragm [2]. Symptoms of patients may be varied depending on location and size of tumor. In addition to compression symptoms such as cough and shortness of breath, however there may be extrapulmonary symptoms such as hypoglycemia and pulmonary osteohypetrophy [1]. We aimed to present a patient who had been operated for laryngeal cancer before being with an undiagnosed mass. We observed that the mass is originated from right diaphragm and it was compatible with SFT histopathology after the surgery we did for both diagnosis and treatment.
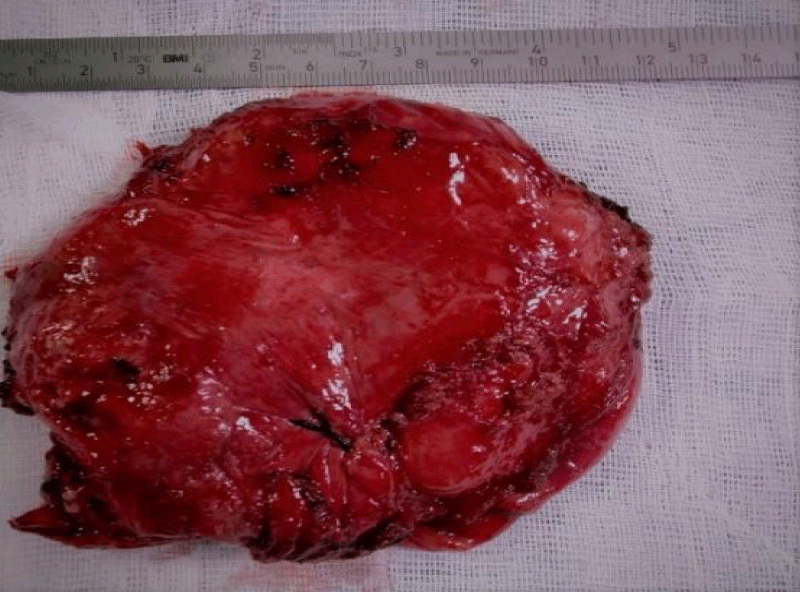
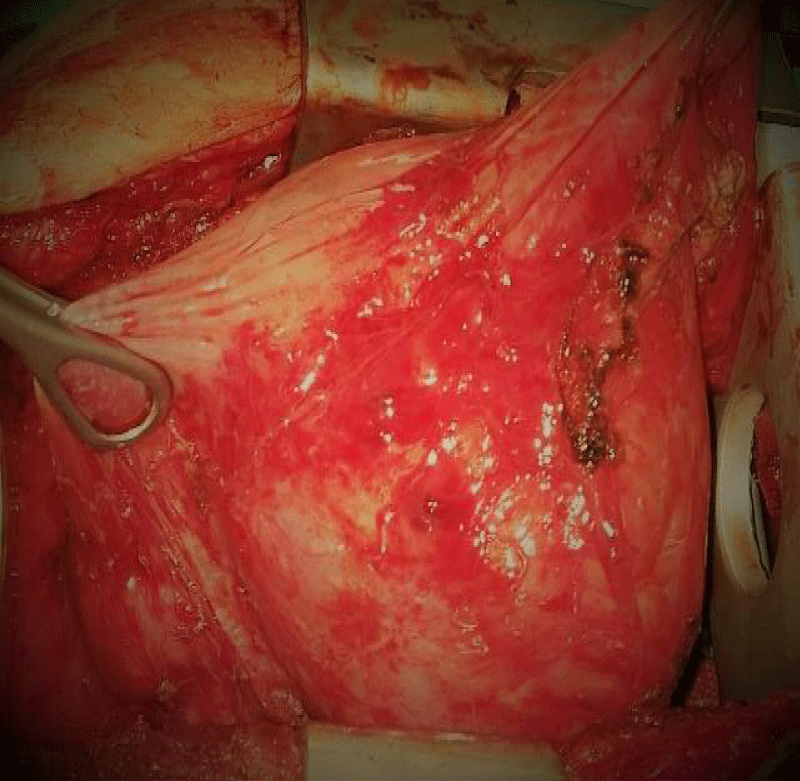
A 61-year-old male patient with tracheostomy due to known laryngeal cancer was referred to our clinic with an undiagnosed lesion with a diameter of approximately 10 cm under the lower lobe of the right lung. The new onset of dyspnea symptom was thought to be primarily due to tracheostomy. However, in the radiological examinations performed, an image of a mass was observed in the right thorax which was close to the diaphragm, a well-circumscribed with different densities was observed in the right lung. No significant anemia or leucocytosis was observed in laboratory values, infection parameters were observed to be within normal limits. Surgical resection was planned for diagnose and also for treatment. We chose to perform a thoracotomy since the mass might have been too large volumed to be manipulating for a thorachoscopic approach. In peroperative observation, the mass was explored in thorax cavity protruding from right diaphragm as well as with adhering to the lower lobe however any pedicle formation was not observed. We performed total surgical excision with safe margins. The mass was histopathologically reported as ‘solitary fibrous tumor’ and the patient discharged from our clinic on the 4th postoperative day. The patient, who is in the 17th month of follow-up, is being followed up without any problem (Figures 1-4).
Figure 1: The image of the totally excised mass.
Figure 2: The image of the totally excised mass.
Figure 3: The right diaphragmatic lesion in thoracic CT.
Figure 4: The pathological view, in 10 X 10, dyed with Hematoxylin & Eosin.
SFT is a rare type of neoplasm of mesenchymal origin, but especially mostly originated from the submesothelial connective tissue of pleura. Although SFTs most commonly occur in the pleura but may also originated from diaphragma, numerous extra pleural sites of involvement have been reported [1].
Our case is valuable giving the fact that its being diaphragmatic originated. And diaphragmatic origin is far less than SFTs of pleural based, furthermore there are less than 5 reported cases in literature for past two decades [2].
SFTs are predominantly observed in middle-aged men and women, with no significant sex predilection [3]. Nevertheless, most tumors are benign, but minority of cases might have aggressive behaviors, such as local recurrence and metastasis [3]. SFTs has been observed at almost every extra pleural anatomic site, including the liver, kidney, pancreas, prostate and breast [3]. Even though video-thoracoscopy approaches were enhanced, still one of the ports had to be enlarged due to size of tumors. Even though there is no consensus about surgical approaches, Takahama, et al. and and Schmid, et al. reported that for SFTs of the pleura with pedicles, thoracoscopic surgery might be preferred, however, if the larger tumor’s diameter is larger than 10 cm, open surgery shoud be performed [4,5]. In this case, the tumor was 10 cm and could not be distinguished from the diaphragm radiologically, thus we should have considered that large adhesion areas would be within possibility.
SFTs are considered as a benign neoplasm due to their slowly growing and low-metastatic rate. Nonetheless malignant types do occur. Even though classification of SFTs are still confusing, according to the World Health Organization Classification of Soft Tissue Tumors, the main features include hypercellularity, significant cellular atypia, tumor necrosis, 4 mitoses among 10 high-power fields, and infiltrative margins defines malignancy in these tumors [6]. And there are also cases reported with metastasis and recurrences [6].
As the tumor grows, the patients show compression symptoms such as cough, pain, dyspnea, corresponding pulmonary osteoarthropathy, and also there are few cases with exhibition of paraneoplastic syndrome and hypoglycemia caused by insulin-like growth factor (ILGF). The association of SFT and hypoglycemia has been defined as ‘Doege-Potter Syndrome’ in literature.
Transthoracic needle biopsy or thoracoscopic biopsy can be helpful in diagnosis, nevertheless the mass must be totally resected for definitive diagnose. Because of the tumors histopathological variability biopsies may have a limited place in diagnosis. That is why total surgical resection is stil the main approach for both diagnosis and treatment. Radiologically, SFTs show well-defined, homogeneous mass which can be pre-diagnosed on chest radiography or computed tomography (CT). Doppler ultrasound, magnetic resonance imaging (MRI), and positron emission tomography (PET) may be helpful in differential diagnosis. In malignant cases, increased 18F-fluorodeoxyglucose (18-FDG) uptake was shown [7].
The prognosis is usually good for benign SFTs. However, because of the different histopathological variation, long‐term follow‐up is necessary. Studies has shown that surgical resection is necessary. If positive surgical margins exist, adjuvant therapies are recommended even though their contribution is still controversial [7]. And our patient is in the 17th month of follow-up and he is being followed up without any problem.
Solitary fibrous tumor of the pleura is an uncommon neoplasm which considered as benign but also may have malignant features. Even in the case of recurrence, the main treatment remains as total surgical excision. Videothoracoscopic approaches is still improving because of giving the fact that SFTs are usually detected when they are large enough to cause compression symptoms. That is the main reason why we chose thoracotomy even though our center has enough experience on videothoracoscopic approaches. Our case is happened to be valuable since it is one of the rare cases which originated from diaphragm. Regardless of the surgical approaches, all SFTs should be respected and the patients should have long follow-ups due to the possibility of recurrence.
- Liu X, Zhu W, Zhou X, Yao H, Su J, et al. 18F-FDG PET/CT imaging findings of multiple solitary fibrous tumor: A case report. Medicine. 2019; 98: e16743. PubMed: https://pubmed.ncbi.nlm.nih.gov/31393388/
- Liu D, Wang Y, Zheng Y, Zhang H, Wang Z, et al. Massive malignant solitary fibrous tumor of the diaphragm: A case report. Medicine. 2020; 99: e18992. PubMed: https://pubmed.ncbi.nlm.nih.gov/32000437/
- Fan J, Qiu J, Wei Q. Extremely rare case of intravascular solitary fibrous tumour in the inferior vena cava with review of the literature. Diagn Pathol. 2019; 14: 86. PubMed: https://pubmed.ncbi.nlm.nih.gov/31391089/
- Takahama M, Kushibe K, Kawaguchi T. Kimura M, Taniguchi S, et al. Video-assisted thoracoscopic surgery is a promising treatment for solitary fibrous tumor of the pleura. Chest. 2004; 125: 1144-1147. PubMed: https://pubmed.ncbi.nlm.nih.gov/15006980/
- Schmid S, Csanadi A, Kaifi JT, Kimura M, Taniguchi S. Prognostic factors in solitary fibrous tumors of the pleura. J Surg Res. 2015; 195: 580–587. PubMed: https://pubmed.ncbi.nlm.nih.gov/15006980/
- Lv G, Wang K, Li M, Li Z, Zheng A, et al. Recurrence of multiple metastases after surgical removal of a primary malignant solitary fibrous tumor from the main bronchus: A case report. Medicine. 2018; 97. e13560. PubMed: https://pubmed.ncbi.nlm.nih.gov/30558017/
- Yanik F, Karamustafaoglu YA, Yoruk Y. Surgical outcomes and clinical courses of solitary fibrous tumors of pleura. Niger J Clin Pract. 2019; 22: 1412-1416. PubMed: https://pubmed.ncbi.nlm.nih.gov/31607732/