More Information
Submitted: February 20, 2024 | Approved: March 18, 2024 | Published: March 19, 2024
How to cite this article: Gazzah H, Hadrich Z, Tlili Y, Hafsi M, Hajri M, et al. Large Cystic Dilatation of the Common Bile Duct. Arch Surg Clin Res. 2024; 8: 009-010.
DOI: 10.29328/journal.ascr.1001077
Copyright License: © Gazzah H, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Congenital cystic dilatation; Common bile duct; Total resection
Large Cystic Dilatation of the Common Bile Duct
Houda Gazzah, Zied Hadrich, Yassine Tlili, Montacer Hafsi*  , Mohamed Hajri and Sahir Omrani
, Mohamed Hajri and Sahir Omrani
Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine of Tunis, Tunisia
*Address for Correspondence: Montacer Hafsi, Department of General Surgery, Mongi Slim University Hospital, Faculty of Medicine of Tunis, Bardo 2000, Tunisia, Email: [email protected]; [email protected]
We report the case of a 57-year-old woman, with no medical or surgical history with a BMI of 32 kg/m², who consulted for paroxysmal pain in the right hypochondrium that appeared a few months ago. Her general condition has not been affected.
Abdominal examination and laboratory liver tests were normal.
On hepatic MRI, cystic dilatation of the common bile duct (type Ia according to Todani Classification) with vesicular lithiasis was detected. The dilatation extended from the hepatic hilum downwards to the cephalic region of the pancreas and measured 80 mm in height and 67 mm in diameter (Figure 1).
Figure 1: Fibrohyalinized tissue with lymphangiectasis.
The patient underwent laparotomic surgery; In comparison to the laparoscopic approach, laparoscopy is feasible despite not having the appropriate technical platform or expertise to perform it, especially given the extensive dilation; we have chosen laparotomy.
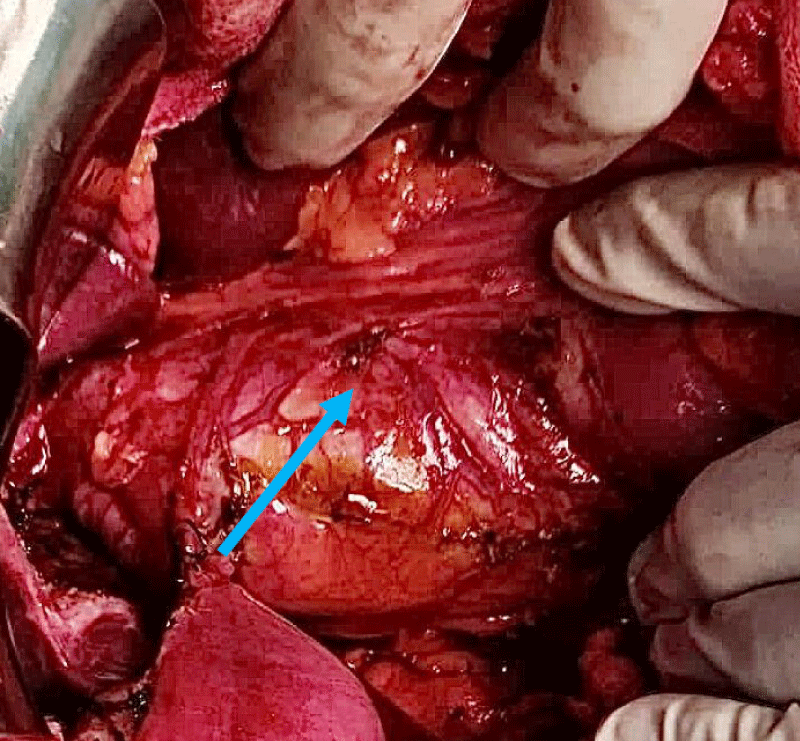
Intraoperatively, a 7 cm cystic mass was discovered that occupied the entire common bile duct (Figure 2).
Figure 2: An intraoperative view showing the cystic dilatation of the common bile duct (blue arrow).
A cholecystectomy, total resection of the common bile duct, and bilio-digestive anastomosis were performed.
The operative follow-up was unfavourable, marked by a massive pulmonary embolism, which ultimately resulted in the death of our patient.
Congenital cystic dilatation of the bile ducts is a rare condition that primarily affects women [1].
The Todani classification of bile duct cysts divides choledochal cysts into five groups [2]. It provides strategic orientation for management.
An abnormality of the biliary-pancreatic junction, often associated with type I dilatation, as in our case, is believed to promote carcinogenesis [3].
Complete surgical excision is the preferred treatment [4].
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Ethical approval
Not applicable. Our institution requires no ethical approval for case reports.
- Li B, Chen BW, Xia LS. The Initial Experience of Laparoscopic Management for Type VI Choledochal Cyst in Children. J Laparoendosc Adv Surg Tech A. 2024 Mar;34(3):280-283. doi: 10.1089/lap.2023.0229. Epub 2023 Oct 16. PMID: 37844069.
- Dumitrascu T, Lupescu I, Ionescu M. The Todani classification for bile duct cysts: an overview. Acta Chir Belg. 2012 Sep-Oct;112(5):340-5. doi: 10.1080/00015458.2012.11680849. PMID: 23175921.
- Dutta S, Jain A, Reddy A, Nelamangala Ramakrishnaiah VP. Anomalous Pancreaticobiliary Duct Junction in an Unusual Case of Synchronous Gallbladder and Bile Duct Malignancy. Cureus. 2021 Feb 13;13(2):e13331. doi: 10.7759/cureus.13331. PMID: 33738174; PMCID: PMC7959653.
- Xia HT. Standardized Surgical Management for Cystic Dilation of the Bile Ducts Based on Clinical and Pathological Studies: A Narrative Review. Gastroenterol Res Pract. 2020 Sep 15;2020:3432786. doi: 10.1155/2020/3432786. PMID: 33014038; PMCID: PMC7512076.