More Information
Submitted: March 01, 2024 | Approved: April 01, 2024 | Published: April 02, 2024
How to cite this article: Islam SR, Paul D, Sarkar SA, Emon MH, Ahmed T. CVS: An Effective Strategy to Prevent Bile Duct Injury. Arch Surg Clin Res. 2024; 8: 027-031.
DOI: 10.29328/journal.ascr.1001080
Copyright License: © Islam SR, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Bile duct injury; Laparoscopic cholecystectomy; Critical view of safety; Infundibular technique
Abbreviations: LC: Laparoscopic Cholecystectomy; CVS: Critical View of Safety; BDI: Bile Duct Injury; GB: Gall Bladder; IN: Infundibulum
CVS: An Effective Strategy to Prevent Bile Duct Injury
Sardar Rezaul Islam1*, Debabrata Paul2, Shah Alam Sarkar3, Mohammad Hanif Emon4 and Tania Ahmed4
1Professor & Head, Department of Surgery, Ad-din Women’s Medical College Hospital (AWMCH), Bangladesh
2Associate Professor, Department of Surgery, Jahurul Islam Medical College Hospital (JIMCH), Bangladesh
3Assistant Professor, Department of Surgery, JIMCH, Bangladesh
4Assistant Professor, Department of Surgery, AWMCH, Bangladesh
*Address for Correspondence: Sardar Rezaul Islam, MBBS, FRCSEd, FACS, HOD, Professor & Head, Department of Surgery, Ad-din Women’s Medical College Hospital (AWMCH), 2, Boro mogbazar, Dhaka-1217, Bangladesh, Email: [email protected]; [email protected]
Background: Bile duct injuries have been substantially increased after the introduction of laparoscopic cholecystectomy (LC). These are accompanied by major morbidity and mortality. Studies have shown varying degrees of success in the reduction of bile duct injury (BDI) using the Critical View of Safety (CVS) technique. The aim of this study was to see the efficacy of the CVS technique as the sole method of dissection in laparoscopic cholecystectomy.
Methods: 1647 cases of LC were done between January 2012 and January 2022 for a period of 10 years in two hospitals. All were operated by the CVS dissection technique and none by the infundibular technique. Cases included acute cholecystitis, chronic cholecystitis, gangrenous cholecystitis, empyema, and Gallbladder (GB) polyp.
Results: The average operating time was 42 minutes and the range was 13 to 80 minutes. In 92% of cases, all 3 criteria of CVS were achieved. In the remaining 8% cases were either converted to open or operated by a division of GB or subtotal cholecystectomy was done. There was only one case of cystic duct stump leak requiring drainage and common bile duct stenting.
Conclusion: The excellent outcome of our study suggests that the CVS method will be the gold standard technique in the dissection of the gallbladder in LC. Further dissemination of the technique is necessary to improve safety in LC.
Bile duct injury (BDI) is the most serious iatrogenic complication in Laparoscopic Cholecystectomy (LC). The incidence of major BDI is 0.1 to 0.5%. The most common cause of serious BDI is misidentification. A method of identification of cystic structures was first introduced by Steven Strasberg in the USA in 1992. Later he named it Critical View of Safety (CVS) in 1995. We were inspired by Professor Michael Brunt, a colleague of Professor Strasberg, through his lecture and meeting him at several surgical conferences.
Three criteria are needed to achieve CVS:
➢ Hepato-cystic triangle is cleared of fat and fibrous tissue,
➢ The lower third of the gall bladder (GB) is dissected off the cystic plate,
➢ Two and only two structures are seen entering the GB which are the cystic duct and cystic artery.
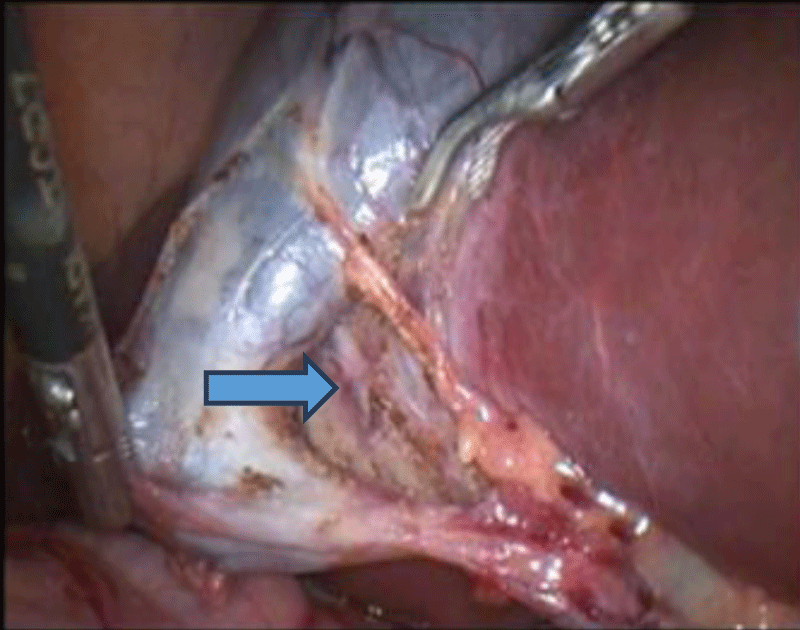
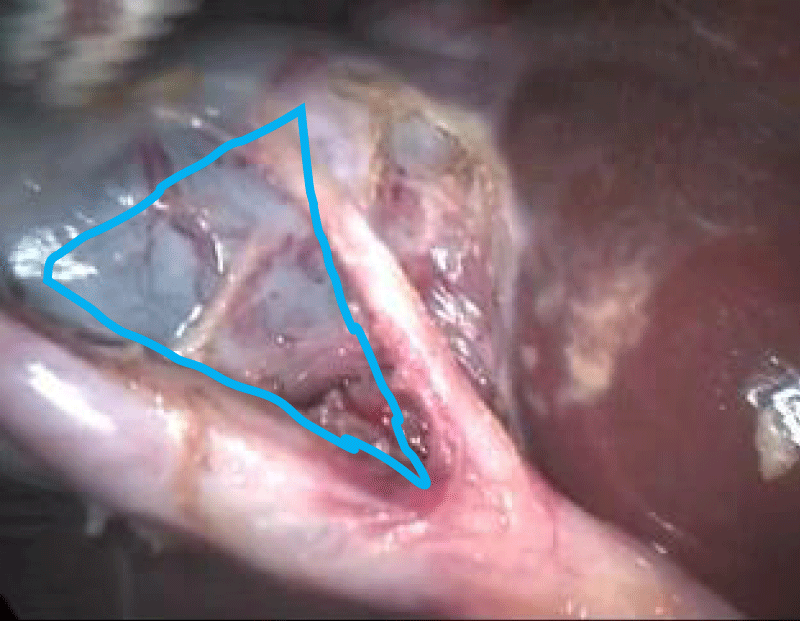
Some surgeons have adopted this CVS method for dissection for LC. Others use the classical infundibular (IN) method or both. Professor Strasberg mentioned that in his early experience, he had considerable difficulty taking the gallbladder off the cystic plate completely without first dividing the cystic duct and artery [1]. The gallbladder tended to twist on the cystic structures after it was totally freed from its attachments to the liver just like open cholecystectomy. This resulted in difficulty in clipping and dividing the cystic artery and duct. In the course of time, it was realized that the same identification of cystic structures was obtained by taking the gallbladder off the lower third of the cystic plate, leaving the fundal part of the gallbladder attached to the liver. In addition, the twisting problem, which occurred when the gallbladder was detached completely, does not occur when the fundus of the gallbladder remained attached. At that point, the question became what was the least amount of gallbladder that must be separated from the cystic plate to achieve the identification of cystic structures. It was agreed that a whitish cystic plate should be clearly visible in the window between the cystic artery and the cystic duct (Figure 1). Only then the cystic artery and cystic duct be safely clipped and divided [2].
Figure 1: CVS anterior view, Cystic plate is visible.
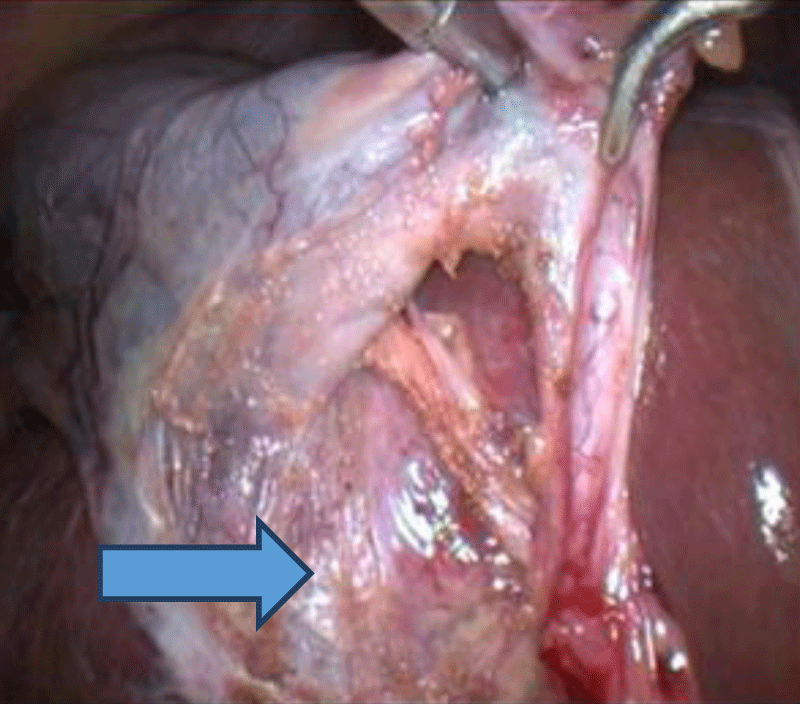
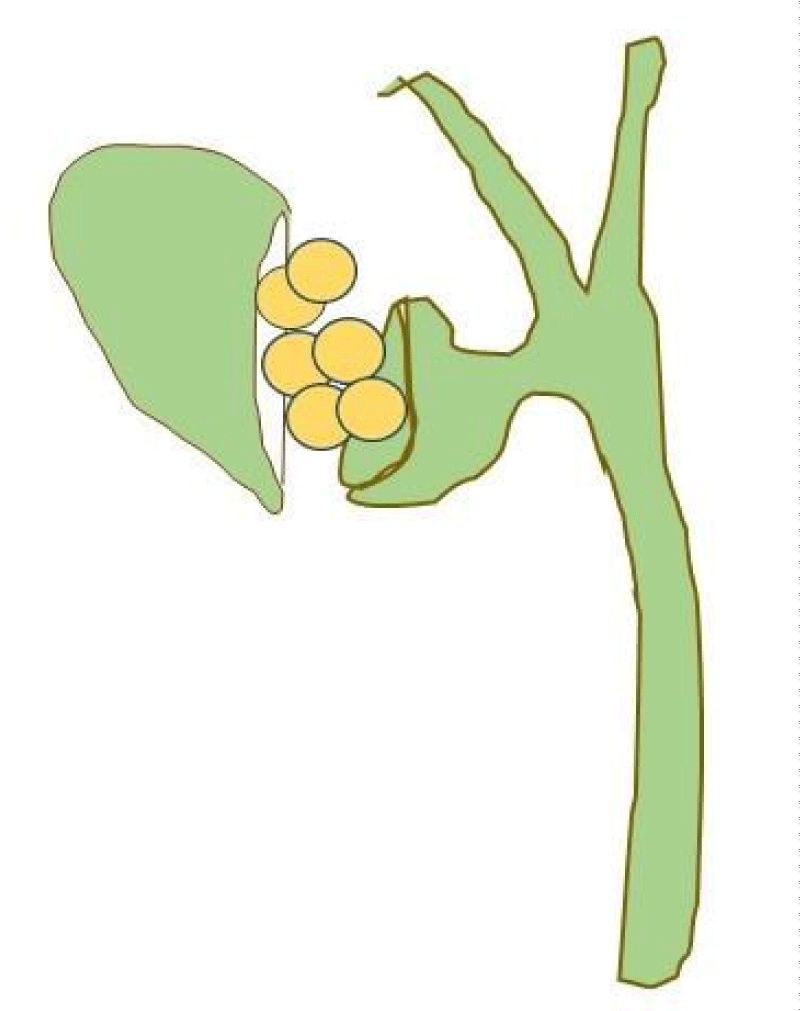
When CVS cannot be attained, there are several bailout strategies such as a cholecystostomy, subtotal cholecystectomy removes the free wall of the gallbladder and ablates the mucosa but does not close the gallbladder remnant. Conversion to open procedure can always be done in a situation of extreme adhesion, or obscure anatomy with a sepsis-like empyema or gangrenous GB, provided an expert surgeon for open surgery is available in the center (Figure 2).
Figure 2: CVS posterior view (cystic plate).
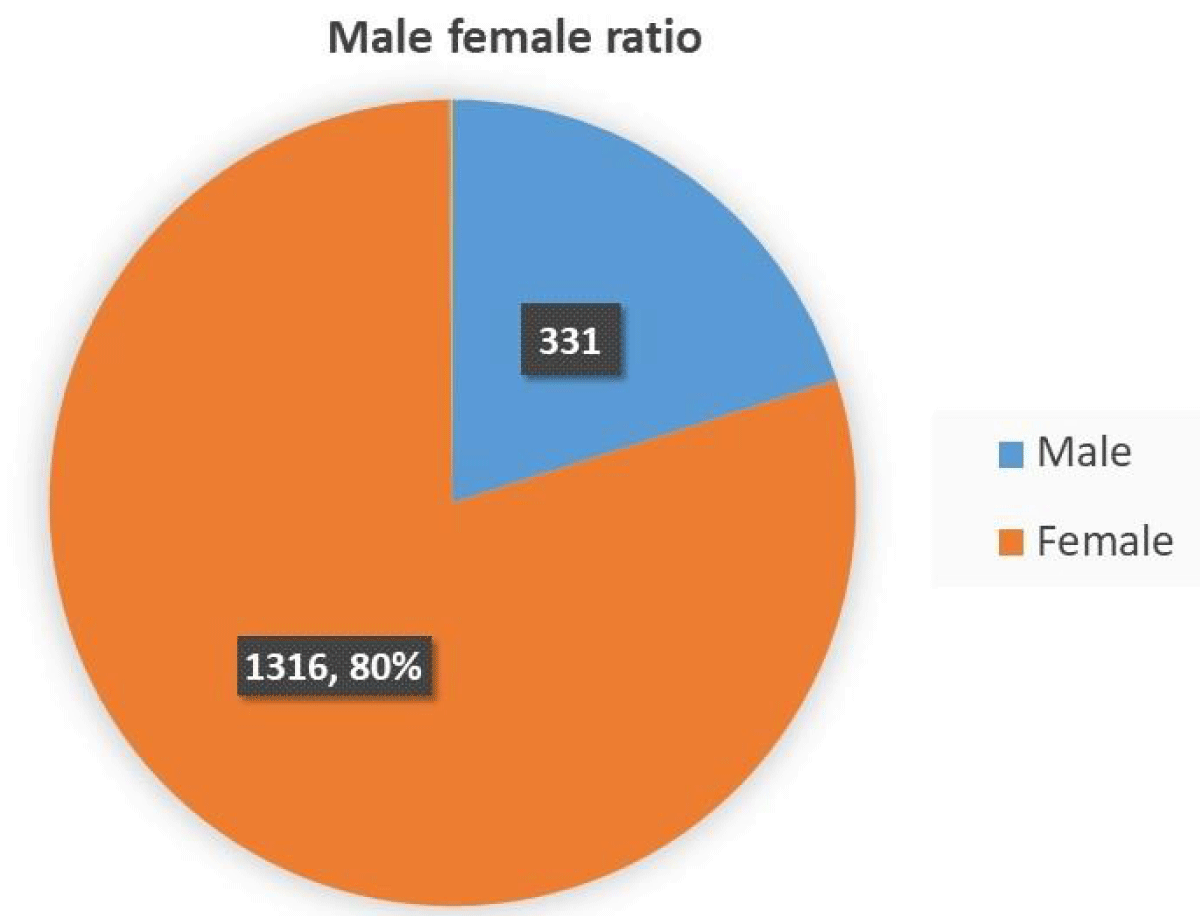
1647 cases of LC were done between January 2012 and January 2022 in Jahurul Islam Medical College and Ad-din Women’s Medical College Hospital by the first author. All patients were operated on by CVS dissection technique and none by infundibular technique. Data were collected in a retrospective manner. Patients were admitted both through outpatient and emergency departments. The age of the patients was from 2 years to 87 years. Male female ratio was 1:4. Cases included acute cholecystitis, mucocele, empyema, chronic cholecystitis, and GB polyp. Any patients with unstable hemodynamic conditions or severe lung disease were excluded from the study. Conventional 4 ports were used. Two 10mm ports were placed on the umbilicus and epigastrium. Two 5 mm ports were placed on the mid-clavicular line and anterior axillary line. The fundus of the GB was pushed cranially by the anterior axillary port.
CVS dissection technique
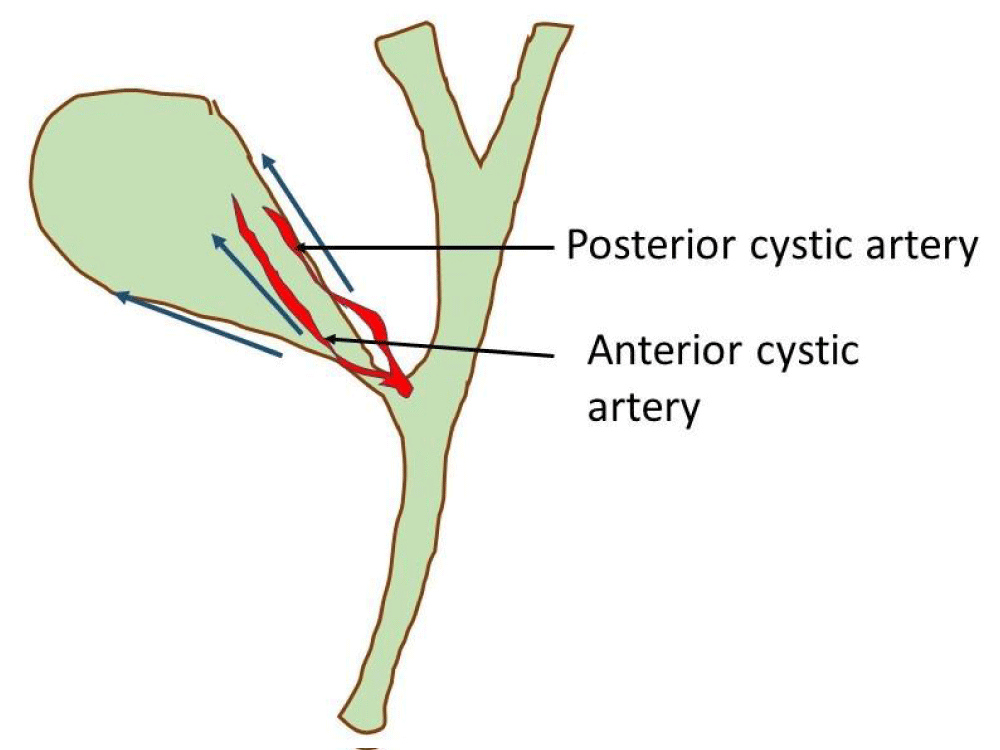
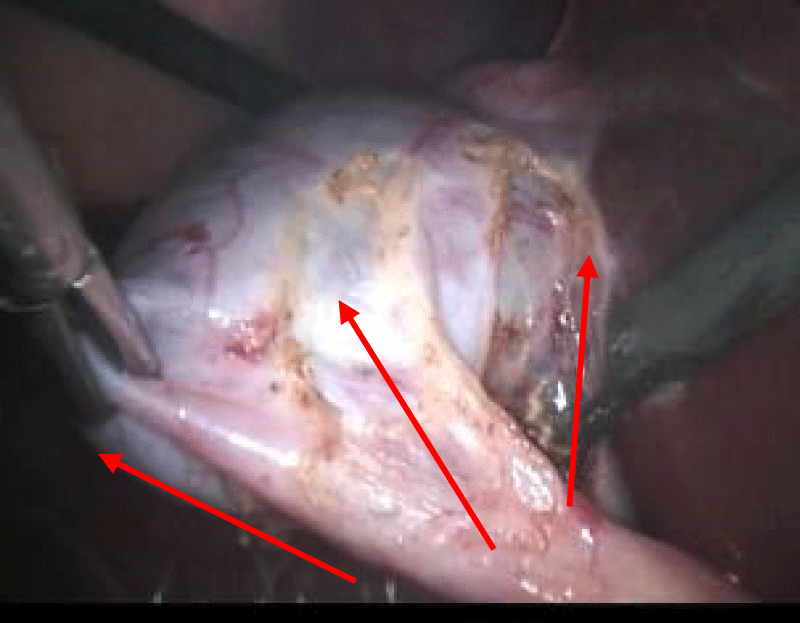
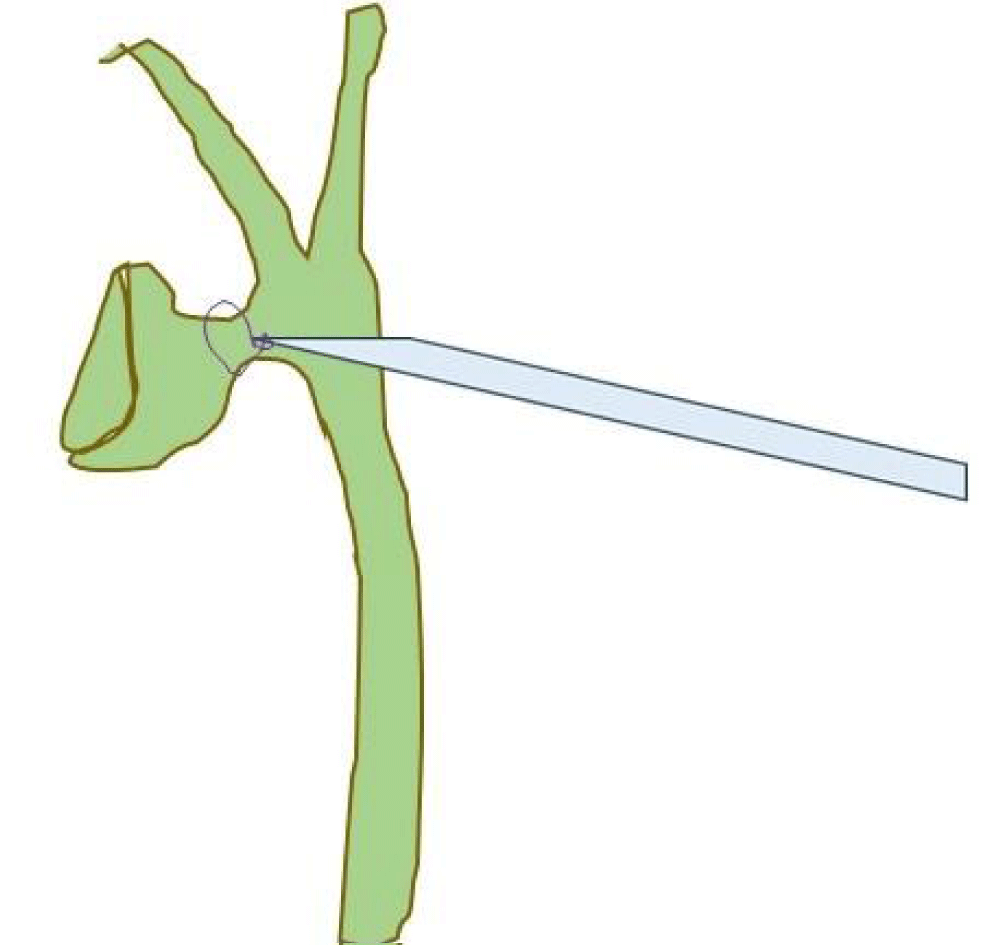
In the dissection of the GB, we used the 111 technique (Figures 3,4). The first incision of the serosa is performed both on the right and left hepato-cystic groove and extends upwards almost to the fundus. Low power diathermy (18 to 20) was used for these incisions. These incisions join each other to make a window behind the GB. Dissection is done on the lateral aspect of the anterior cystic artery and Calott’s node with hook diathermy also. This step helps to gain access to the critical safety triangle. The critical safety triangle is defined as a triangle between the gallbladder wall on the right, the cystic duct inferiorly, and the cystic artery on the left. Then mobilization of the infundibulum, both anteriorly and posteriorly was done by teasing fats and fibrous tissue around the neck of the GB with Maryland forceps. This permits visualization of the cystic plate through the triangle, well above Ruviers’ sulcus (Figures 5-7). The cystic artery and the cystic duct are then clipped separately and divided. Afterward, retrograde dissection of the gallbladder completes the operation.
Figure 3: 111 technique of CVS method.
Figure 4: 111 technique./p>
Figure 5: Safety triangle.
Figure 6: Steps in difficult GB.
Figure 7: Endo-loop around the neck in swollen cystic duct.
Summary of conventional steps of CVS:
➢ Cephalad traction of the fundus
➢ Lateral traction on the infundibulum
➢ Dissection at the Medial and lateral border of the infundibulum
➢ Dissection towards the fundus
➢ An incision on the lateral aspect of the anterior cystic artery
➢ Enter the triangle of safety
➢ Anterior and posterior dissection around the infundibulum-
➢ Visible liver surface through the triangle of safety
➢ Achievement of CVS
➢ Clipping of cystic duct and artery.
In difficult gallbladder
➢ Early division of the anterior cystic artery
➢ Then posterior dissection
Or
➢ Divide the GB on the body
➢ Remove stones by an endo-bag
➢ Remove the fundus with stone
➢ Complete dissection behind the neck of the GB
➢ Clip or ligate the cystic duct
➢ Excise the remnant of the GB
Or
➢ Subtotal cholecystectomy.
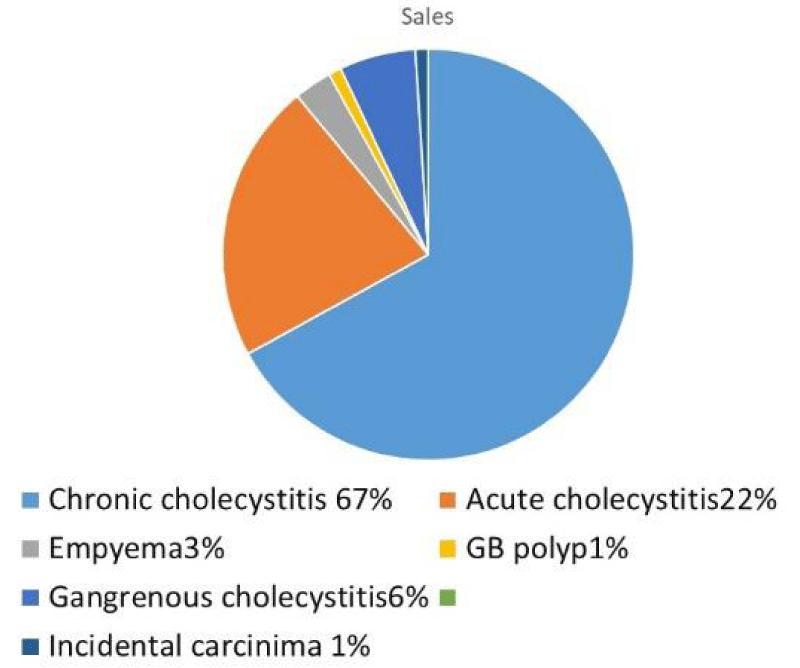
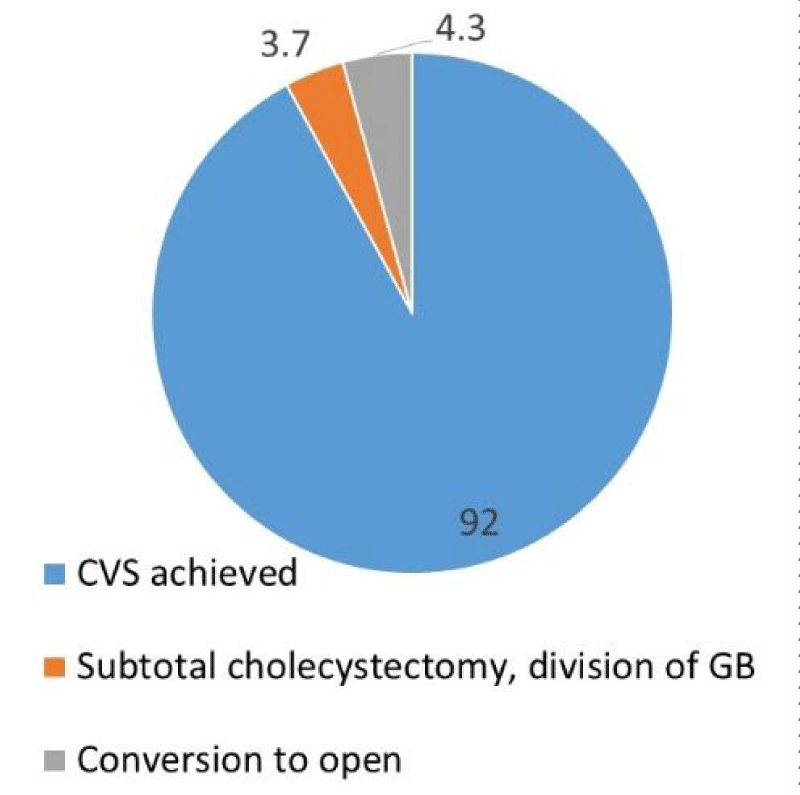
The average operating time was 42 minutes and the range was 13 to 80 minutes. All 3 criteria of CVS were achieved in 1515 (92%) cases out of 1647 cases. Male female ratio was 1:4 (Diagram 1). These 8% cases were operated either by dividing the GB, subtotal cholecystectomy or converted to open. Cystic structures were never clipped without posterior dissection of the GB from the cystic plate. There was no postoperative death in our series. Our rate of conversion was 4.3%. There was one incidence of postoperative bile leak, which required drainage and stenting of the CBD (0.06%). There was no major bile duct injury requiring bile duct reconstruction. The histopathology of the GB specimen was analyzed and plotted in Diagram 2.
Diagram 1: Male-female ratio.
Diagram 2: Pattern of histopathology of GB.
Surgeons have long strived to make LC the safest and complication-free procedure. This effort has been made successful to some extent by the introduction and application of CVS [3,4]. In our study the operative time is significantly reduced for patients with CVS technique, which is 42 minutes. Vettoretto et al. and Viswanathan V also found a significant reduction in operating time (51.5 min), which is comparable to our study [5,6]. Another important aspect pointed out by Lam T and Manatakis DK in separate studies is that there is negligible difference in achieving adequate CVS scores with operator experience (consultant vs. trainees) without adding significant operative time in the hands of trainees. Thus this technique is advocated for teaching as it is largely safe regardless of surgeons' experience [7,8]. Although the CVs technique may have a little more chance of bleeding as involves dissection of the lower third of the GB while cystic artery supply is still intact. By practicing the art of the CVS technique for a period of time incidence of bleeding is minimized.
In our series 8% of cases, CVS could not be achieved. The reason is in these cases calot’s triangle had dense adhesion and distorted anatomy. Examples are severe acute Gangrenous cholecystitis, empyema GB, and Mirizzi syndrome. In these cases either GB was divided, subtotal cholecystectomy or converted to open to avoid inadvertent bile duct injury (Diagram 3). In some cases where the cystic artery intimately adhered with the cystic duct, clip or endo-loop ligature was applied to the duct and artery combinedly after cystic plate dissection.
Diagram 3: Outcome of the procedure.
There was no mortality in our series. Morbidity including minor bile leaks requiring stenting was only 0.06%. However, there was no incidence of major bile duct injury requiring bile duct reconstruction. This finding is superior to many published series, where the rate of major BDI in LC was 0.1% to 0.5% [5,9-11].
Currently, the CVS technique is accepted as a Gold Standard for the reduction of morbidity and mortality associated with LC by the European Association of Endoscopic Surgery (EAES) [12-14]. There are no randomized controlled trials published up-to-date to give us level-1 evidence that CVS prevents bile duct injuries. The average bile duct injury reported before the era of CVS was 3-4 per 1000 cases of LC. The event rate is so low that a randomized trial involving a huge number of samples was not feasible. However, if we look at the large case series published so far, we believe that major BDI can be prevented by strictly adhering to all three criteria of CVS [15-18]. The reason is in the CVS method cystic structures are not divided before dissection of the lower third of the GB. This gives a very clear visualization of the cystic duct and cystic artery. Hence this method reduces the chance of mis-identification of cystic structures. Even after more than 20 years, many surgeons have a poor understanding of the criteria for CVS, especially those who were not taught CVS during residency [19,20]. Reluctance to adopt new techniques or methods can also be a challenge.
Although the “critical view of safety” requires more dissection as compared to the infundibular technique, once learned and mastered, it is a faster and safer identification technique during laparoscopic cholecystectomy. To prove that the CVS dissection method prevents bile duct injury required a randomized trial involving a large number of samples. The excellent outcome of our study forecasts that the CVS method is the gold standard technique in the dissection of the gallbladder in LC. Further dissemination of the technique is necessary to improve safety in LC.
- Steven M. Strasberg A perspective on the critical view of safety in laparoscopic cholecystectomy. Annals of Laparoscopic and Endoscopic Surgery. doi: 10.21037/ales.2017.04.08
- Strasberg SM, Pucci MJ, Brunt LM, Deziel DJ. Subtotal Cholecystectomy-"Fenestrating" vs "Reconstituting" Subtypes and the Prevention of Bile Duct Injury: Definition of the Optimal Procedure in Difficult Operative Conditions. J Am Coll Surg. 2016 Jan;222(1):89-96. doi: 10.1016/j.jamcollsurg.2015.09.019. Epub 2015 Oct 9. PMID: 26521077.
- Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the "critical view of safety" technique. J Gastrointest Surg. 2009 Mar;13(3):498-503. doi: 10.1007/s11605-008-0748-8. Epub 2008 Nov 14. PMID: 19009323.
- Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. 2008 Oct;74(10):985-7. PMID: 18942628.
- Vettoretto N, Saronni C, Harbi A, Balestra L, Taglietti L, Giovanetti M. Critical view of safety during laparoscopic cholecystectomy. J Soc Laparoendosc Surg. 2011; 15(3):322. doi:10.4293/108680811X13071180407474.
- Viswanathan V, Garg HP. Critical view of safety technique during laparoscopic cholecystectomy in prevention of biliary injuries. Int J Int Med Res. 2016; 3(4):35–40.
- Lam T, Usatoff V, Chan ST. Are we getting the critical view? A prospective study of photographic documentation during laparoscopic cholecystectomy. HPB (Oxford). 2014 Sep;16(9):859-63. doi: 10.1111/hpb.12243. Epub 2014 Mar 17. PMID: 24635851; PMCID: PMC4159460.
- Manatakis DK, Vitalis A, Agalianos C, Terzis I, Kyriazanos ID, Davides D. Teaching and learning the critical view of safety technique in laparoscopic cholecystectomy. HPB. 2016; 18:e664–e665. doi:10.1016/j. hpb.2016.01.007.
- Nuzzo G, Giuliante F, Giovannini I, Ardito F, D'Acapito F, Vellone M, Murazio M, Capelli G. Bile duct injury during laparoscopic cholecystectomy: results of an Italian national survey on 56 591 cholecystectomies. Arch Surg. 2005 Oct;140(10):986-92. doi: 10.1001/archsurg.140.10.986. PMID: 16230550.
- Waage A, Nilsson M. Iatrogenic bile duct injury: a population-based study of 152 776 cholecystectomies in the Swedish Inpatient Registry. Arch Surg. 2006 Dec;141(12):1207-13. doi: 10.1001/archsurg.141.12.1207. PMID: 17178963.
- Martin D, Uldry E, Demartines N, Halkic N. Bile duct injuries after laparoscopic cholecystectomy: 11-year experience in a tertiary center. Biosci Trends. 2016 Jul 19;10(3):197-201. doi: 10.5582/bst.2016.01065. Epub 2016 Jun 17. PMID: 27319974.
- Eikermann M, Siegel R, Broeders I, Dziri C, Fingerhut A, Gutt C, Jaschinski T, Nassar A, Paganini AM, Pieper D, Targarona E, Schrewe M, Shamiyeh A, Strik M, Neugebauer EA; European Association for Endoscopic Surgery. Prevention and treatment of bile duct injuries during laparoscopic cholecystectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2012 Nov;26(11):3003-39. doi: 10.1007/s00464-012-2511-1. Epub 2012 Oct 6. PMID: 23052493.
- Kaya B, Fersahoglu MM, Kilic F, Onur E, Memisoglu K. Importance of critical view of safety in laparoscopic cholecystectomy: a survey of 120 serial patients, with no incidence of complications. Ann Hepatobiliary Pancreat Surg. 2017 Feb;21(1):17-20. doi: 10.14701/ahbps.2017.21.1.17. Epub 2017 Feb 28. PMID: 28317041; PMCID: PMC5353907.
- Almutairi AF, Hussain YA. Triangle of safety technique: a new approach to laparoscopic cholecystectomy. HPB Surg. 2009;2009:476159. doi: 10.1155/2009/476159. Epub 2009 Jun 17. PMID: 19547662; PMCID: PMC2699444.
- Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. 2008 Oct;74(10):985-7. PMID: 18942628.
- Heistermann HP, Tobusch A, Palmes D. Der ''Sicherheits-Blic'' als Beitrag zur Risikoreduktion bei der laparoskopischen Cholezystektomie [Prevention of bile duct injuries after laparoscopic cholecystectomy. "The critical view of safety"]. Zentralbl Chir. 2006 Dec;131(6):460-5. German. doi: 10.1055/s-2006-957031. PMID: 17206564.
- Misra M, Schiff J, Rendon G, Rothschild J, Schwaitzberg S. Laparoscopic cholecystectomy after the learning curve: what should we expect? Surg Endosc. 2005 Sep;19(9):1266-71. doi: 10.1007/s00464-004-8919-5. Epub 2005 Jul 21. PMID: 16021365.
- Sanjay P, Fulke JL, Exon DJ. 'Critical view of safety' as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg. 2010 Aug;14(8):1280-4. doi: 10.1007/s11605-010-1251-6. Epub 2010 Jun 10. PMID: 20535578.
- Daly SC, Deziel DJ, Li X, Thaqi M, Millikan KW, Myers JA, Bonomo S, Luu MB. Current practices in biliary surgery: Do we practice what we teach? Surg Endosc. 2016 Aug;30(8):3345-50. doi: 10.1007/s00464-015-4609-8. Epub 2015 Nov 5. PMID: 26541721.
- Chen CB, Palazzo F, Doane SM, Winter JM, Lavu H, Chojnacki KA, Rosato EL, Yeo CJ, Pucci MJ. Increasing resident utilization and recognition of the critical view of safety during laparoscopic cholecystectomy: a pilot study from an academic medical center. Surg Endosc. 2017 Apr;31(4):1627-1635. doi: 10.1007/s00464-016-5150-0. Epub 2016 Aug 5. PMID: 27495348.